25 Dec 2025
- 15 Comments
When you pick up a generic pill from the pharmacy, you assume it works just like the brand-name version. But what happens when that pill sits on a shelf for months-or years? Not all generic drugs degrade the same way. And when they do, it’s not just about losing potency. It’s about safety.
What Does Shelf Life Really Mean?
Shelf life isn’t just a date printed on the bottle. It’s the period during which a drug maintains its chemical structure, physical form, and microbial safety under specific storage conditions. The U.S. Food and Drug Administration (FDA) requires that every medication-brand or generic-must prove through scientific testing that it stays within strict limits for purity, strength, and safety until that expiration date.Think of it like milk. If you leave milk out at room temperature, it sours. It doesn’t just taste bad-it becomes unsafe. The same principle applies to drugs. A tablet might look fine, but inside, the active ingredient could be breaking down into harmful byproducts. Or the coating might crack, letting moisture in and triggering bacterial growth.
The International Council for Harmonisation (ICH) set the global standard with Q1A(R2) in 2003. It says: test your drug under real-world conditions. That means storing samples at 25°C and 60% humidity for up to 36 months. For accelerated testing, you crank it up to 40°C and 75% humidity for six months. But here’s the catch: accelerated testing doesn’t always predict real-life degradation.
Why Generic Drugs Are Different
Generic drugs are cheaper because they don’t repeat the expensive clinical trials of the original. But they still need to match the brand in active ingredient, dosage, and absorption. What they don’t have to match? The exact excipients-the fillers, binders, and coatings that hold the pill together.That’s where things go wrong. A 2020 FDA study found that 17.3% of generic levothyroxine products had stability issues not seen in Synthroid. Why? Moisture. The generic versions used different coatings that didn’t block humidity as well. Over time, the hormone degraded. Patients didn’t get the right dose. Some ended up with uncontrolled thyroid levels, weight gain, fatigue, or worse.
It’s not just levothyroxine. Insulin pens, antibiotics, and even heart medications have shown similar problems. One quality assurance professional on the American Pharmaceutical Review forum lost $250,000 and 18 months when their accelerated test showed no degradation-but real-time storage revealed crystallization at 24 months. The culprit? A polymorphic transition. That’s when the drug’s molecular structure changes under mild heat and humidity, something accelerated tests often miss.
Four Types of Degradation You Can’t Ignore
Stability testing looks at four key areas:- Chemical stability: Is the active ingredient breaking down? High Performance Liquid Chromatography (HPLC) detects impurities. ICH Q3B says unknown impurities must stay below 0.1%. If they rise, you’ve got a toxic risk.
- Physical stability: Does the pill still dissolve properly? Does a liquid still flow? For nanoparticles-like those used in cystic fibrosis treatments-particles must stay under 200nm. If they clump together, they can’t reach the target cells. One Texas A&M study showed a 90% drop in effectiveness when particles grew beyond that size.
- Microbiological stability: Is mold or bacteria growing? Non-sterile products must stay under 100 colony-forming units per gram (CFU/g). Preservatives can fail if water activity changes. In fact, 41.3% of stability-related recalls in 2022 were due to preservative breakdown.
- Functional stability: Does the delivery system still work? A metered-dose inhaler must deliver 90-110% of the labeled dose. If the valve clogs or the propellant leaks, the patient gets nothing.
Each of these requires validated methods. And validation isn’t optional. Only 58.4% of companies do it right, according to PDA data. That’s a red flag.
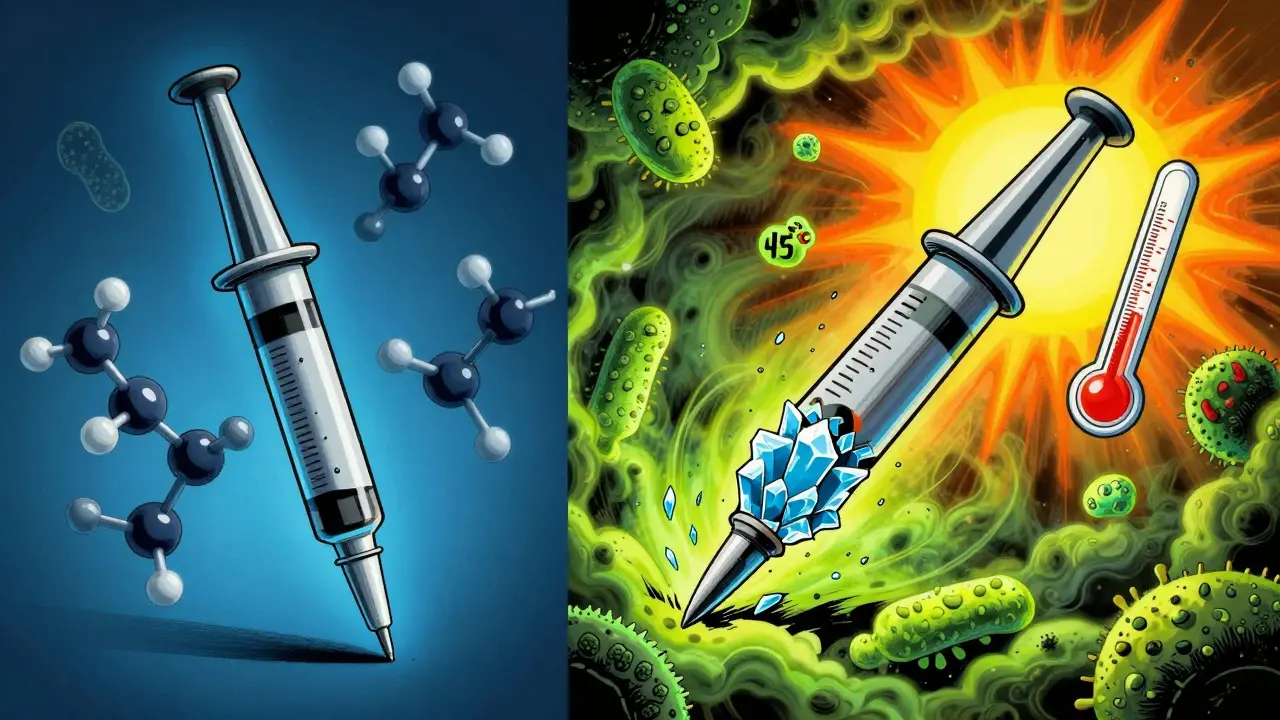
Storage Conditions Are a Silent Killer
You’ve seen the label: “Store at room temperature.” But what does that even mean? The FDA defines it as 15-30°C (59-86°F). Research shows 24-25°C is the sweet spot for testing. But in the real world? A garage in Arizona hits 45°C in summer. A warehouse in India might not have AC. A patient keeps their pills in the bathroom-hot, steamy, humid.And here’s the kicker: 80% of FDA Form 483 observations (official warning notices) for stability failures are about poor storage documentation. Saying “room temperature” isn’t enough. You need to log actual temperature and humidity data. Every single day. Not just once a week. Not just when you feel like it.
Low-income countries face even bigger risks. The WHO found 28.7% of medicines there fail stability tests-not because of bad manufacturing, but because of broken cold chains. No refrigeration. No climate control. Just heat, dust, and time.
What’s Changing in 2025?
The game is shifting. ICH Q12, effective since late 2023, lets companies make post-approval changes to stability protocols without reapplying for approval. That’s a big deal. It means faster innovation-but also more responsibility.Companies are now using predictive modeling. The IQ Consortium found that risk-based stability programs cut time-to-market by over 8 months. One pilot with Amgen and Merck shaved 30% off testing time. But regulators still don’t fully trust them. Why? Because many models rely on data from high-heat stress tests that don’t reflect real degradation pathways.
Meanwhile, the FDA’s Continuous Manufacturing Stability Testing (CMST) pilot showed a 40% faster way to determine shelf life for drugs made in continuous production lines. That’s a future-proof method. But it’s still experimental.
And then there’s climate change. A 2022 MIT study projected that by 2050, rising global temperatures could shorten average drug shelf life by 4.7 months. Warehouses in Sydney, Houston, or Mumbai will hit 30°C more than 87 days a year. That’s beyond the “room temperature” range. What happens to your blood pressure meds then?

What You Should Do
If you’re a patient:- Check the expiration date. Don’t use expired meds. Ever.
- Store pills in a cool, dry place-not the bathroom, not the car, not the windowsill.
- If your generic drug seems less effective, talk to your pharmacist. Ask if it’s the same formulation as the brand.
If you’re a manufacturer or pharmacist:
- Don’t rely on accelerated testing alone. Validate with real-time data.
- Monitor storage conditions with digital loggers-not handwritten notes.
- Test for polymorphic changes, especially with drugs prone to crystallization.
- For generics, compare excipients to the reference product. Small differences matter.
And if you’re in regulatory or quality control? Stop cutting corners. The cost of a recall isn’t just financial. It’s human.
Final Thought: Safety Isn’t Optional
Stability testing isn’t paperwork. It’s a lifeline. A single degraded tablet can mean a child doesn’t get enough asthma medication. A diabetic doesn’t get the right insulin dose. A heart patient has a stroke because their blood thinner broke down.The science is there. The regulations are clear. The data is real. What’s missing is consistent execution. And that’s where the risk lives-not in the lab, but in the storage cabinet.
Can generic drugs expire faster than brand-name ones?
Yes. While generics must match the brand in active ingredient and absorption, they can use different fillers, coatings, and manufacturing processes. These differences can make them more sensitive to heat, humidity, or light. A 2020 FDA study found 17.3% of generic levothyroxine products degraded faster than Synthroid due to poor moisture protection.
Is it safe to take expired medication?
It’s not recommended. While most expired drugs don’t turn toxic, they lose potency. A weakened antibiotic might not kill an infection. An expired epinephrine auto-injector might not save a life. The FDA says expiration dates are set to guarantee safety and effectiveness-so don’t risk it.
What causes drugs to degrade?
Four main factors: heat, moisture, light, and oxygen. Chemical breakdown happens when molecules react with water or air. Physical changes include tablets cracking or liquids clouding. Microbial growth occurs if preservatives fail. And for complex drugs like nanoparticles, clumping can render them useless.
How do regulators test drug stability?
They use long-term testing (24-36 months at 25°C/60% RH) and accelerated testing (6 months at 40°C/75% RH). They measure chemical purity with HPLC, physical form with dissolution and particle size tests, microbial safety with CFU counts, and functional performance like dose accuracy. All methods must be validated per ICH Q2(R1).
Why do some stability tests fail even when the product looks fine?
Because degradation isn’t always visible. A tablet can look perfect but have 15% less active ingredient. A liquid might look clear but have bacterial contamination. A capsule might seal fine but leak moisture slowly over months. That’s why labs use precise instruments-not your eyes.
Are there alternatives to traditional stability testing?
Yes-predictive modeling and risk-based approaches are emerging. Companies like Amgen and Merck have used these to cut testing time by 30%. But regulators still require real-time data to back them up. ICH Q12 now allows more flexibility, but full acceptance is still growing.
How does climate change affect drug shelf life?
A 2022 MIT study projected that by 2050, rising global temperatures could reduce average drug shelf life by 4.7 months. Warehouses in major distribution hubs will exceed 30°C for more than 87 days a year-beyond the safe storage range. This threatens supply chains, especially in low-income countries with poor refrigeration.
What should I do if I suspect my generic drug isn’t working?
Don’t stop taking it without talking to your doctor. But do ask your pharmacist: Is this the same formulation as the brand? Could storage conditions have affected it? If symptoms changed after switching generics, it’s worth investigating. Some patients report better results with different manufacturers.


Joanne Smith
December 26, 2025So let me get this straight-we’re trusting our lives to pills that might be sitting in a hot garage in Arizona, and the FDA just says ‘eh, it’s within range’? 🤦♀️
My grandma’s blood pressure med looked fine. Tasted fine. Until she started fainting. Turned out the coating cracked, moisture got in, and the whole thing turned into chemical soup. No one told her. No one checked. Just assumed.
Generic? Sure. But ‘same as brand’? Only if you ignore the fillers that turn into little molecular landmines under humidity. It’s not conspiracy-it’s chemistry. And we’re all just guinea pigs in a warehouse.
And don’t even get me started on the ‘store at room temperature’ label. My bathroom is a sauna. My car is a solar oven. My fridge? Too cold. So where the hell am I supposed to put it? The moon?
Someone needs to start labeling meds like milk. ‘Expires in 6 months. If it smells like regret, don’t take it.’
Ryan Cheng
December 26, 2025This is such an important post-and honestly, so under-discussed.
Most people think expiration dates are just a legal formality, but the science behind degradation is wild. That 17.3% levothyroxine stat? That’s not a glitch-it’s a pattern. And it’s not just thyroid meds. I’ve seen insulin pens go bad in unrefrigerated clinics overseas.
The real issue? We treat drugs like commodities, not life-saving tools. A pill isn’t a can of beans. You can’t just shove it in a box and forget it.
Pharmacists, if you’re reading this: ask patients where they store their meds. Don’t assume. Ask. And if they say ‘the bathroom,’ gently freak out. It’s not rude-it’s lifesaving.
Also, predictive modeling is the future, but we need more real-world validation. Accelerated tests lie sometimes. Trust the data, not the speed.
Ellie Stretshberry
December 28, 2025i just took my meds this morning and thought about this
my bottle says store at room temp but my apartment is always hot
and the pills look fine so i just keep taking them
but now im scared
what if theyre not working
and i dont even know
thanks for making me think about this
maybe i should move them to the kitchen
or something
idk
Zina Constantin
December 29, 2025As someone who grew up in a country where medicine was stored in a cardboard box under a mosquito net, I can tell you-this isn’t just theory. It’s survival.
My aunt took expired antibiotics for her fever. She didn’t die. But she got sepsis anyway. Because the drug didn’t kill the bacteria-it just made it stronger.
And yeah, generics? Sometimes they’re the only option. But we need transparency. Not just ‘same active ingredient.’ We need to know what’s holding it together. What’s the coating? What’s the humidity tolerance?
And if your country doesn’t track storage temps? That’s not negligence. That’s a human rights issue.
Every pill should come with a QR code that shows its journey-from lab to shelf. Not because we’re paranoid. Because we’re human.
Jay Ara
December 30, 2025in india we dont even get proper storage
pharmacies keep medicines in open shelves
no ac no cooler just sun and dust
and still we take them
because no choice
but yeah some generics really dont work same as brand
my friend took generic for epilepsy and had seizures
switched back to brand and boom fine
so its not just placebo
its real
and no one cares
we just hope for the best
Kuldipsinh Rathod
December 30, 2025my cousin died because her heart med stopped working
they said it was expired
but she stored it in the fridge
so how
turns out the generic used a different coating
and the cold made it crack
so it leaked
no one knew
no one tested
just assumed
its scary
we need better standards
not just for rich countries
SHAKTI BHARDWAJ
December 31, 2025OH MY GOD YOU ACTUALLY THINK THE FDA GIVES A SHIT ABOUT YOU?
THEY’RE OUT HERE LETTING PHARMA COMPANIES SLIP BY WITH ACCELERATED TESTS THAT ARE AS USEFUL AS A TISSUE IN A HURRICANE
AND YOU’RE SITTING THERE WORRYING ABOUT YOUR BATHROOM?
THEY’RE MAKING BILLIONS WHILE YOU’RE TAKING CRACKED PILLS LIKE A GOOD LITTLE SHEEP
THEY WANT YOU WEAK. THEY WANT YOU DEPENDENT. THEY WANT YOU TO THINK ‘OH WELL I’LL JUST TAKE ANOTHER’
WHEN THE REAL PROBLEM IS THEY’RE SELLING YOU CHEAP PLASTIC WITH A BRAND NAME ON IT
STOP BEING A VICTIM. START ASKING FOR THE REAL FORMULA
OR STAY SICK. I DONT CARE
david jackson
January 2, 2026Let me tell you about the time I spent 18 months trying to debug a stability failure in a nanoparticle-based asthma inhaler.
Everything looked perfect. Accelerated tests? Clean. HPLC? Perfect. Dissolution? On the nose.
Then, after 24 months of real-time storage in a warehouse in Atlanta-bam. Particles clumped. Size jumped from 180nm to 420nm. Effectiveness? Down 92%.
Why? Polymorphic transition. A silent, invisible shift in molecular structure. Like ice turning to steam without boiling.
The FDA didn’t even require that test. The manufacturer didn’t think it mattered. The patients? They just got worse.
And now? I don’t trust any drug unless I know the excipient profile. Because it’s not the active ingredient that kills you.
It’s the invisible glue holding it together.
And we’re all just walking blindfolded through a minefield labeled ‘safe’.
Jody Kennedy
January 2, 2026My dad’s diabetes meds expired last year. He kept taking them because he didn’t want to spend the money on a new prescription.
He didn’t die. But his HbA1c shot up to 11.5. He was exhausted. Blurry vision. He thought it was just aging.
We switched to a different generic-same active ingredient, different coating. Within 3 weeks, his numbers were back in range.
It wasn’t placebo. It wasn’t coincidence.
It was chemistry. And it was hidden.
So if your generic isn’t working like it used to? Don’t blame yourself. Don’t blame the disease.
Blame the filler. And ask your pharmacist: ‘Is this the same as the brand?’
They’ll know. If they care.
christian ebongue
January 3, 2026my last generic blood pressure med made me dizzy
switched back to brand
instantly better
so yeah
they’re not all the same
and no one tells you
lol
jesse chen
January 3, 2026It’s not just about degradation-it’s about trust. We’ve been conditioned to believe that ‘generic’ means ‘equivalent,’ but the truth is, equivalence is measured in a lab under perfect conditions, not in a humid closet in Florida.
And when your body reacts differently to a generic? You’re not ‘sensitive.’ You’re not ‘imagining it.’ You’re experiencing real, measurable differences in bioavailability, coating integrity, and excipient behavior.
It’s not paranoia. It’s pharmacology.
So if you feel off after switching? Speak up. Demand the manufacturer’s name. Ask for the batch number. Check the storage history.
Because your life isn’t a cost-cutting exercise.
It’s a biological system. And systems fail when you ignore their variables.
Prasanthi Kontemukkala
January 4, 2026i live in a small town in india and we get generics because thats all we can afford
but i’ve noticed some batches work better than others
so i started writing down the manufacturer name
now i ask for the same one every time
its not about brand loyalty
its about survival
and honestly
if more people did this
companies would have to care
because we’d stop buying the bad ones
simple as that
Alex Ragen
January 5, 2026Ah, the sacred altar of pharmaceutical capitalism-where efficacy is a footnote and profit is the only sacrament.
How poetic that we’ve reduced human physiology to a variable in a cost-benefit analysis, where a polymorphic transition is merely an ‘unforeseen variance’ and a child’s asthma attack is a ‘statistical outlier.’
ICH Q12? A neoliberal Trojan horse. Letting corporations self-regulate stability like a wolf guarding the henhouse.
And climate change? It’s not a ‘threat’-it’s a revelation. The planet is finally screaming back at our hubris.
Perhaps the real degradation isn’t in the pill-but in our collective moral architecture.
And yet, we still trust the label.
How tragically, beautifully, horrifyingly human.
Lori Anne Franklin
January 7, 2026i just moved and my meds got left in the car for a week in july
they looked fine so i kept taking them
now im wondering if i messed up my thyroid
im so sorry i didnt know
but now i know
so i put them in a drawer
no more bathroom
no more car
and i’m gonna ask my pharmacist next time
thank you for making me care
i didnt even think about this before
david jackson
January 7, 2026Just read the comment from the Texas A&M guy about polymorphic transitions. That’s exactly what happened in my lab. The accelerated test showed zero change. Real-time storage? Crystallization at 24 months. We missed it because we were chasing speed, not truth.
And now I’m thinking-how many patients are taking pills that look perfect but are chemically broken?
It’s not just generics. It’s every drug that’s been stored in a warehouse with no humidity control.
Maybe we need a ‘drug health tracker’-like a Fitbit for your meds. Log temperature, humidity, location. Scan the bottle. Get alerts.
Because if we can track our sleep and steps, why can’t we track whether our lifesaving pills are still alive?