21 Feb 2026
- 0 Comments
When a pharmacist swaps a brand-name drug for a generic version, it’s not just a simple switch. Behind that decision is a web of legal, clinical, and administrative steps - and documentation is the backbone of it all. In Australia, as in many countries, this isn’t optional. It’s a critical safety measure that protects patients, ensures compliance, and keeps the healthcare system running smoothly.
Generic substitution means dispensing a different brand or unbranded version of a drug that’s been approved as therapeutically equivalent to the one prescribed. This practice has been around for decades, driven by cost savings and proven safety. In the U.S., nearly 90% of prescriptions filled are for generics. But even when a generic is just as effective, the rules around documenting that switch vary - and getting it wrong can lead to errors, insurance denials, or even patient harm.
What Exactly Must Be Documented?
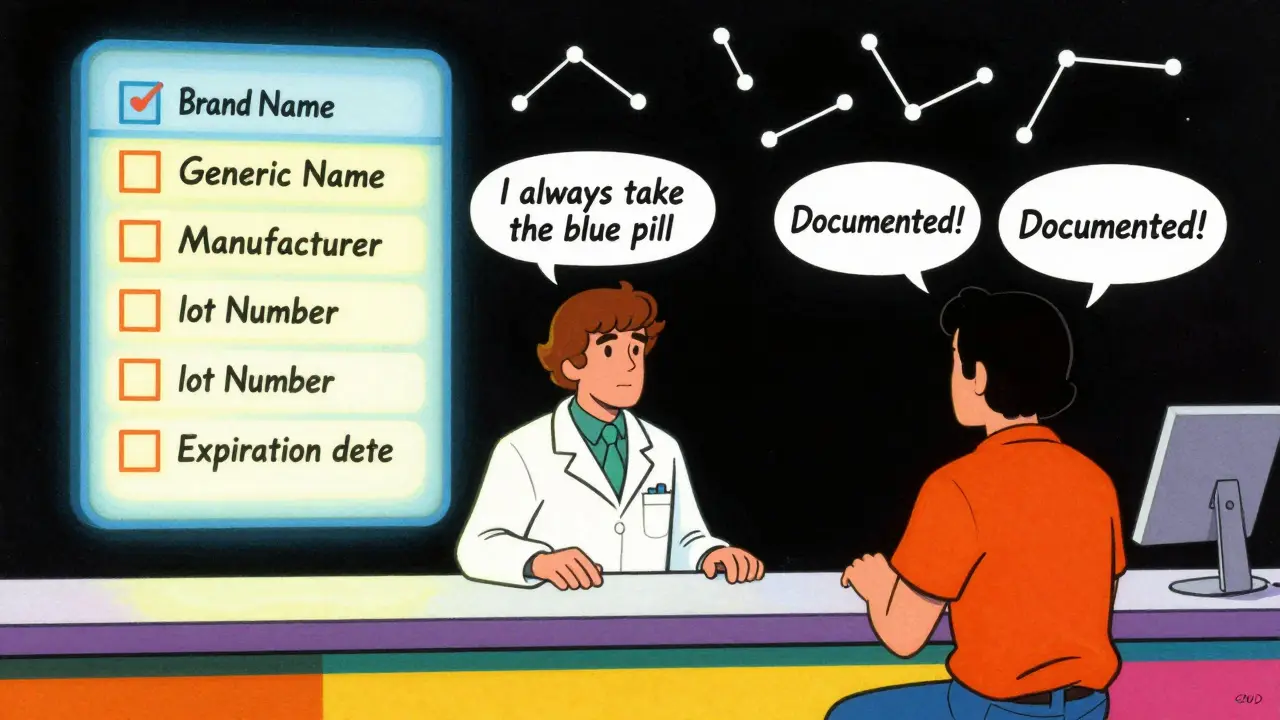
Pharmacists don’t just need to note that a substitution happened. They need to record the specifics. Most jurisdictions require at least five key pieces of information:
- The brand-name drug prescribed by the doctor
- The generic name of the drug dispensed
- The manufacturer of the generic product
- The lot number
- The expiration date
These aren’t just bureaucratic checkboxes. Each one serves a purpose. The lot number and expiration date help track recalls or expired stock. The manufacturer matters because different companies produce generics with slightly different inactive ingredients - and those can affect patients with allergies or sensitivities. If a patient has a reaction, this data can be traced back in hours, not days.
Some states and countries go further. For example, in Australia, the Therapeutic Goods Administration (TGA) requires that substitution records be retained for at least two years. In the U.S., 48 states mandate the same five elements. But in places like Oklahoma, pharmacists must also prove they had permission from the prescriber or patient before making the swap. In California, starting January 2024, substitutions must be documented electronically in real time - and the prescriber gets an automatic notification.
When Is Substitution Allowed - And When Is It Forbidden?
Not every drug can be swapped. The biggest red flag is a narrow therapeutic index (NTI) drug. These are medications where even a tiny change in blood level can cause serious harm. Think warfarin, lithium, or levothyroxine. Even though the FDA considers generics bioequivalent, clinical experience shows that switching NTI drugs can lead to dangerous fluctuations. That’s why 17 U.S. states require extra steps: physician approval, patient consent, and detailed documentation.
And it’s not just about NTI drugs. If a doctor writes “Dispense as Written” or “Do Not Substitute” on the prescription, pharmacists must follow that instruction - no exceptions. In fact, the World Medical Association recommends that once a patient is stable on a specific brand - especially for chronic conditions like epilepsy or hypertension - any switch should require the prescriber’s explicit approval.
Some patients also have strong preferences. A 2022 survey of Australian pharmacists found that 1 in 5 patients asked specifically for the brand they’d been using. In those cases, the pharmacist must document the patient’s request, even if the generic is cheaper. Patient autonomy matters - and so does the paper trail.
Why Documentation Matters More Than You Think
It’s easy to think of documentation as busywork. But it’s not. It’s a safety net.
Consider this real case: A 68-year-old man on warfarin was switched to a generic version without proper documentation. His INR levels spiked, leading to internal bleeding and a hospital stay. The pharmacy’s records showed the substitution happened - but not which manufacturer’s generic was used. Without that detail, doctors couldn’t trace whether the issue was with the drug, the batch, or the patient’s metabolism. The hospital had to run expensive tests and delay treatment.
On the flip side, a 2022 study across 150 community pharmacies showed that when substitution decisions were fully documented, medication errors dropped by 17.3%. Why? Because when a pharmacist reviews a patient’s history and sees that a previous substitution led to dizziness or nausea, they can flag it before it happens again.
Insurance companies also rely on this data. If a claim is denied because the generic wasn’t properly recorded, the pharmacy loses money - and the patient might not get their meds. One pharmacist in Sydney told me, “I’ve lost three claims this month because I forgot to enter the lot number. It took 10 minutes each time to fix. Now I have a checklist on my screen.”
How Technology Is Changing the Game
Most pharmacies now use electronic systems - but not all are built the same. A 2023 report from Epic Systems found that 32% of pharmacies using their software needed custom tweaks just to meet state or local documentation rules. That’s because there’s no universal standard.
Some systems auto-fill the generic name but leave the lot number blank. Others don’t even have a field for manufacturer. That’s where pharmacists have to step in - manually adding details, double-checking entries, and sometimes printing out forms to attach to the patient’s file.
The good news? New tools are emerging. Australia’s Pharmaceutical Benefits Scheme (PBS) now integrates substitution logs directly into the national e-prescribing system. When a pharmacist dispenses a generic, the prescriber’s portal receives an automatic update. That’s a huge step toward transparency.
Even more promising? Blockchain pilots. A trial by the National Pharmaceutical Council in 2023 showed that using blockchain to track substitutions cut documentation errors by 22%. Every swap is timestamped, immutable, and accessible to authorized providers. It’s not mainstream yet - but it’s coming.

What Pharmacists Need to Know Right Now
If you’re a pharmacist, here’s what you need to do today:
- Know your local laws. Rules vary by state or territory - and they change. Subscribe to updates from your pharmacy board.
- Use a checklist. Even if your system has built-in prompts, a printed or digital checklist ensures nothing slips through.
- Train new staff. Onboarding can take 4-6 weeks just to get comfortable with documentation rules. Don’t assume they know.
- Document patient conversations. If a patient says, “I’ve always taken the blue pill,” write it down. It’s not opinion - it’s clinical history.
- Review records weekly. Spot patterns. If multiple patients report side effects after a certain generic, investigate.
And if you’re a prescriber? Document why you chose a brand-name drug. If it’s because of a past reaction, an allergy, or a patient’s preference - write it down. That information travels with the prescription.
What’s Next for Generic Substitution?
The trend is clear: standardization. Right now, 50 U.S. states have 50 different rules. Australia is moving toward a national framework. The Therapeutic Goods Administration is working with state health departments to align documentation requirements. A draft national guideline is expected in late 2024.
One thing won’t change: the need for clear, accurate records. As generic drugs make up 90% of prescriptions but only 23% of drug spending, the pressure to cut costs will only grow. But cost savings shouldn’t come at the cost of safety. Documentation is how we keep both in balance.
Pharmacists aren’t just dispensing pills. They’re managing risk, protecting patients, and holding the system accountable. And every time they document a substitution - no matter how small it seems - they’re doing something vital.
Do pharmacists need patient consent to substitute a generic drug?
It depends on the jurisdiction. In many places, including most U.S. states and parts of Australia, pharmacists can substitute generics without explicit consent - as long as the prescription doesn’t say "Do Not Substitute." But in some states like Oklahoma and California, patient consent is required by law. Always check local regulations. If a patient asks for their usual brand, document their request - it’s part of their medical history.
What happens if a pharmacist forgets to document a substitution?
The consequences vary. At minimum, the pharmacy may lose reimbursement from insurance providers. In serious cases - especially with NTI drugs like warfarin - inadequate documentation can lead to regulatory fines, disciplinary action from the pharmacy board, or even liability if a patient is harmed. Many pharmacists report that insurance claims are denied within 48 hours if substitution details are missing. That’s why most pharmacies now use automated reminders or mandatory fields in their dispensing software.
Are all generic drugs considered safe to substitute?
Most are - but not all. The FDA and TGA approve generics based on bioequivalence, meaning they deliver the same amount of active ingredient into the bloodstream as the brand. But bioequivalence doesn’t always guarantee identical clinical outcomes. For drugs with a narrow therapeutic index - like lithium, digoxin, or levothyroxine - even small differences can cause problems. Many states require special documentation and physician approval before substituting these. Always check if the drug is classified as NTI before swapping.
How long must substitution records be kept?
In Australia, the Therapeutic Goods Administration requires records to be retained for at least two years. In the U.S., most states require a minimum of two to five years, depending on whether the drug is controlled or non-controlled. Some states, like New York, require five years for all prescriptions. Always follow the strictest rule that applies to your location. Electronic records should be backed up securely and accessible for audits.
Can a prescriber override a pharmacist’s substitution?
Yes - and they often do. If a doctor writes "Dispense as Written," "Brand Necessary," or "Do Not Substitute" on the prescription, the pharmacist is legally required to fill it exactly as written. Some prescribers do this because of past patient reactions, allergies to inactive ingredients, or clinical experience. Pharmacists must honor these instructions. In fact, the American Medical Association recommends that physicians clearly document any medical reason for prescribing a brand-name drug - not just to prevent substitution, but to protect patient safety.

