3 Dec 2025
- 12 Comments
Every morning, millions of people sprinkle turmeric on eggs, stir it into golden milk, or swallow capsules labeled "natural anti-inflammatory." It’s safe, right? After all, it’s just a spice. But if you’re on a blood thinner-warfarin, rivaroxaban, aspirin, clopidogrel, or any other-this common kitchen ingredient could be quietly putting you at risk for a life-threatening bleed.
How Turmeric Acts Like a Blood Thinner
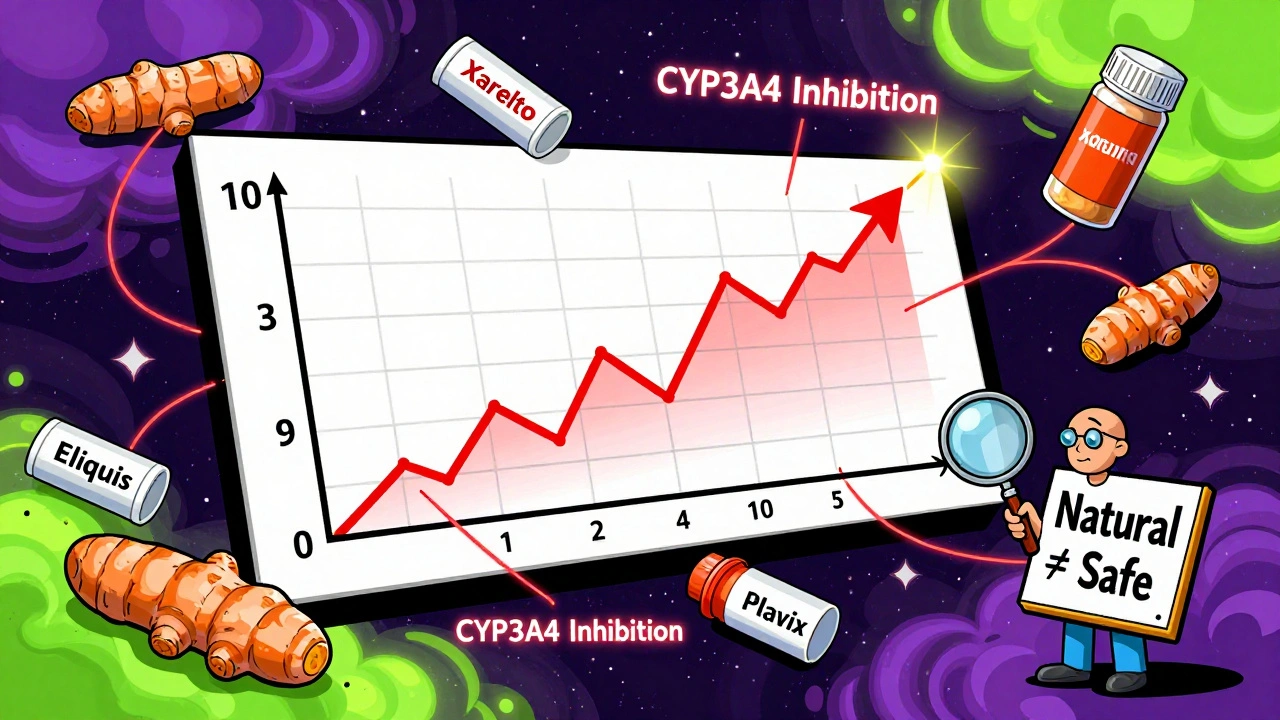
Turmeric gets its bright yellow color from curcumin, and that’s where the problem starts. Curcumin isn’t just a flavoring agent. It’s a powerful biological compound that interferes with your body’s ability to form clots. Research shows it directly inhibits two key clotting proteins: thrombin and factor Xa. These are the same targets of prescription drugs like Xarelto and Eliquis. But unlike those medications, which are dosed precisely and monitored with blood tests, turmeric supplements vary wildly in curcumin content. One capsule might have 5% curcumin. Another might have 95%. There’s no standard.On top of that, curcumin slows down platelet aggregation-the clumping of blood cells that helps seal cuts. This means it doesn’t just thin your blood; it also makes it harder for your body to stop bleeding when you need it to. In a 2012 study published in PubMed, curcumin was found to prolong both prothrombin time (PT) and activated partial thromboplastin time (aPTT), two standard lab tests used to measure clotting speed. The higher the dose, the longer the delay. That’s not a subtle effect. That’s a clinical signal.
The Real-World Danger: When INR Skyrockets to 10+
Numbers don’t lie. The International Normalized Ratio (INR) measures how long it takes your blood to clot. For someone on warfarin, the safe range is 2 to 3.5. Anything above 4.5 is dangerous. Above 6? Emergency territory. And then there’s the case reported by Medsafe New Zealand in 2018: a patient on stable warfarin therapy started taking a turmeric supplement. Within weeks, their INR jumped to over 10. That’s not a typo. That’s more than triple the upper limit of safety.What happened next? The patient faced a serious risk of internal bleeding-possibly even a brain hemorrhage. Survival rates for intracranial bleeds with INR above 10 can be as low as 50%. This wasn’t a theoretical risk. It was a real, documented medical emergency triggered by something many people consider harmless.
It’s Not Just Warfarin-Other Blood Thinners Are Affected Too
Some people think, "I’m on Xarelto or Plavix, not warfarin, so I’m fine." That’s a dangerous assumption. The Welsh Medicines Information Centre (WMIC) confirmed in October 2024 that curcumin can interfere with the clearance of warfarin from the body, but it doesn’t stop there. Curcumin also interacts with direct oral anticoagulants (DOACs) like rivaroxaban and apixaban. It’s not just about clotting proteins-it’s about liver enzymes.Curcumin inhibits CYP3A4, the same enzyme your liver uses to break down many medications. When this enzyme slows down, drugs like tacrolimus (used by transplant patients) build up to toxic levels. In one case, a patient taking 15 spoonfuls of turmeric powder daily developed acute kidney injury and tacrolimus levels more than double the safe limit. That’s not an isolated incident. The same enzyme issue affects clopidogrel, aspirin, and even some antibiotics. If your medication is processed by the liver, turmeric might be changing how fast it works-and not in a good way.
Supplements Are Not Regulated Like Drugs
Here’s the kicker: turmeric supplements aren’t held to the same standards as prescription drugs. The FDA doesn’t test them for purity, potency, or interactions before they hit shelves. A bottle labeled "1,000 mg turmeric" might contain 20 mg of actual curcumin-or 800 mg. You won’t know unless you pay for third-party testing. And even then, most people don’t.Meanwhile, doctors have clear dosing guidelines for warfarin. They adjust your dose based on weekly INR tests. But with turmeric? No lab test can tell you how much is in your system. No doctor can predict how your body will react. That’s why the British Heart Foundation, Mayo Clinic, and Medsafe all warn against combining turmeric with anticoagulants-not because they’re anti-natural, but because the risk is real, measurable, and deadly.
What About Cooking With Turmeric?
If you’re worried about your curry, don’t be. The amount of curcumin in food is too low to cause harm. You’d need to eat over a pound of raw turmeric root daily to reach the doses linked to interactions. That’s not realistic. The real danger comes from concentrated supplements-pills, powders, extracts, tinctures. These are designed to deliver high doses. That’s what overwhelms your system.So enjoy your turmeric latte or rice dish. But if you’re on a blood thinner, skip the capsules. If you’ve already been taking them, don’t stop cold turkey. Talk to your doctor. Abruptly stopping supplements can also cause issues. Your provider needs to monitor your INR and adjust your medication if needed.

What Should You Do?
- If you’re on warfarin, Xarelto, Eliquis, Plavix, aspirin, or any other blood thinner: do not take turmeric supplements.
- Stop all turmeric supplements at least two weeks before any surgery or dental procedure. Bleeding during or after can be catastrophic.
- Don’t assume "natural" means safe. Many deadly interactions come from herbs and supplements, not pharmaceuticals.
- Always tell your doctor and pharmacist about every supplement you take-even if you think it’s "just turmeric."
- If you’ve been taking turmeric and notice unusual bruising, nosebleeds, blood in urine or stool, or severe headaches, seek medical help immediately.
The bottom line: Turmeric isn’t the enemy. But when you’re on a blood thinner, it becomes a hidden hazard. There’s no safe middle ground. Either you take the supplement and risk bleeding-or you don’t. There’s no "maybe" when your life is on the line.
What About Other Medications?
Turmeric doesn’t just play nice with blood thinners. It can also interfere with diabetes medications, causing blood sugar to drop too low. It may reduce the effectiveness of some antidepressants and increase the side effects of drugs like sulfasalazine. In one small study, people taking 2 grams of curcumin daily had 3.2 times higher levels of sulfasalazine in their blood-enough to cause serious side effects. The same enzyme inhibition that affects clotting affects everything else your body metabolizes.If you’re on multiple medications, turmeric isn’t a harmless addition. It’s a wildcard. And in medicine, wildcards are the ones that kill.
Why Do People Still Take It?
Because the marketing is everywhere. "Anti-inflammatory! Antioxidant! Anti-aging!" The claims sound scientific. But science doesn’t say "take this with your blood thinner." It says the opposite. The gap between what people believe and what the evidence shows is widening. And it’s costing lives.Health authorities in New Zealand, the UK, the US, and Australia have all issued warnings. The WMIC updated its guidance in 2024. The Mayo Clinic and British Heart Foundation include turmeric in their official patient advisories. Yet, most people still don’t know.
If you’re reading this, you’re one of the lucky ones. You now know the risk. Share it. Talk to your family. Tell your friends who take warfarin. One conversation could prevent a tragedy.


val kendra
December 4, 2025I’ve been on warfarin for 5 years and took turmeric capsules for "joint pain" for 8 months. One morning I woke up with a black eye and no memory of bumping into anything. My INR was 8.2. Turns out the supplement bottle had 95% curcumin. I didn’t even know it was a problem until my pharmacist screamed at me. Now I only use turmeric in curry. No more pills. Ever.
Jessica Baydowicz
December 6, 2025OMG this is so important!! I just bought a turmeric gummy from Whole Foods thinking it was "healthy". Now I’m terrified. Thanks for the wake-up call!! I’m tossing mine out right now 💪
Joe Lam
December 6, 2025Of course turmeric interferes with anticoagulants. It’s a potent CYP3A4 inhibitor. Anyone who doesn’t know this hasn’t read a single pharmacokinetics paper. The fact that people treat supplements like candy is why medicine is in crisis. You wouldn’t take random pills from a street vendor-why treat your liver like a landfill?
Scott van Haastrecht
December 7, 2025Someone’s gonna die because they thought "natural" meant "safe." And when they bleed out in the ER, their family will blame the doctor. Not the supplement industry. Not the influencers. Not the FDA. Always the doctor. That’s the real tragedy here.
Bill Wolfe
December 8, 2025Let’s be real-people who take turmeric supplements are the same ones who drink celery juice for "detox" and wear crystals to "balance chakras." They don’t care about science. They care about feeling like they’re "doing something" for their health. Meanwhile, their liver is screaming in a language only pharmacists understand. 🤦♂️
Dematteo Lasonya
December 8, 2025I’m a nurse and I’ve seen this too many times. A patient comes in with a GI bleed after taking turmeric with warfarin. They say, "But my yoga instructor said it was good for inflammation." I just nod and call the pharmacy. No judgment. Just facts. Please, if you’re on blood thinners-skip the capsules. Your body will thank you.
Rudy Van den Boogaert
December 8, 2025My dad’s on Xarelto and he’s been taking turmeric for his knees. I just told him this article and he said "I’ll stop tomorrow." I’m so glad I found this. Thanks for writing it.
Gillian Watson
December 10, 2025Interesting that the UK’s NICE guidelines mention this but most GPs still don’t ask about supplements. We talk about statins and antihypertensives but not turmeric. Maybe it’s because it’s "just a spice." But it’s not just a spice when it’s 500mg per capsule. We need better patient education.
Gareth Storer
December 11, 2025So let me get this straight. You’re telling me I can’t have my golden milk latte because some guy in a lab coat says curcumin might do something? Cool. I’ll keep drinking it. I’d rather bleed than live without my morning ritual. 😌
Martyn Stuart
December 11, 2025Important note: Turmeric in food is fine. But supplements? They’re not regulated. The FDA doesn’t require them to list curcumin content. So you could be taking 10x the dose you think. Always check for USP or NSF certification. And if you’re on meds-ask your pharmacist. They’re the real heroes here.
Isabelle Bujold
December 12, 2025I’m a pharmacist in Toronto and I’ve had three patients in the last six months with INRs over 8 because of turmeric supplements. One was an 82-year-old woman who thought it was "better than aspirin." She ended up in the ICU with a subdural hematoma. The supplement bottle? No label. No batch number. Just "Pure Turmeric Extract" on a plastic jar from a website that looked like it was built in 2003. We need better labeling. We need public awareness. And we need doctors to stop assuming patients know what they’re taking.
Chase Brittingham
December 12, 2025This is why I always tell my mom to tell her doctor about every pill, powder, or tea she takes. She’s on Plavix and takes ashwagandha, fish oil, and turmeric. I showed her this and she cried. Not because she was scared-but because she felt guilty for not telling her doctor. We need to normalize saying "I take this supplement" without shame. It’s not weird. It’s smart.