9 Jan 2026
- 10 Comments
When you're stuck in a low mood for weeks-no matter how hard you try to shake it off-you're not just being lazy or negative. You might be dealing with major depressive disorder (MDD). It’s not a phase. It’s not something you can ‘think your way out of.’ And it’s more common than you think: about 1 in 6 U.S. adults experience it each year, according to the National Alliance on Mental Illness. The good news? There are proven ways to treat it. Two of the most effective are antidepressants and psychotherapy. And often, using both together works better than either one alone.
What Major Depressive Disorder Really Feels Like
Major Depressive Disorder isn’t just sadness. It’s a persistent feeling of emptiness, hopelessness, or numbness that lasts for at least two weeks. You might lose interest in things you used to love-hanging out with friends, cooking, even watching your favorite show. Sleep changes. Appetite shifts. Concentration becomes impossible. Some people feel physically heavy, like they’re dragging themselves through molasses. Others feel restless, agitated, or constantly on edge. And yes, some have thoughts about not wanting to be here anymore. That’s not weakness. That’s the illness talking. It doesn’t always start after a bad event. Sometimes, it just shows up out of nowhere. That’s why it’s so confusing for people around you-and for you, too. You might wonder, “Why me? I didn’t do anything wrong.” The truth is, MDD comes from a mix of brain chemistry, life stress, genetics, and even physical health issues. It’s not your fault. And it’s not permanent.Antidepressants: How They Work and What to Expect
If your doctor suggests medication, they’ll likely start with a second-generation antidepressant. These are safer and have fewer side effects than older drugs. The most common are SSRIs-Selective Serotonin Reuptake Inhibitors. Examples include escitalopram, sertraline, and paroxetine. SNRIs, like venlafaxine, are also used, especially if you’re dealing with severe symptoms or chronic pain alongside depression. These medications don’t work like magic pills. You won’t feel better the next day. Most people notice small improvements after one or two weeks, but it takes six to twelve weeks to feel the full effect. That’s why sticking with them is so important-even when you feel worse before you feel better. Some people report increased anxiety or nausea in the first few weeks. That’s common. It usually fades. Side effects are real. Weight gain, sexual dysfunction, trouble sleeping, and emotional blunting (feeling “numb”) are reported by many. But here’s the thing: not everyone gets them. And if you do, your doctor can adjust the dose or switch you to another medication. There are more than a dozen FDA-approved options. Finding the right one is part of the process. For those who don’t respond to medication after trying two or more, electroconvulsive therapy (ECT) is an option. It’s not what you see in old movies. Today, it’s done under anesthesia, with controlled electric pulses. It’s highly effective for severe, treatment-resistant depression. Many people say it gave them their life back.Psychotherapy: The Talking Cure That Actually Works
Talk therapy isn’t just venting. Evidence-based psychotherapy is structured, goal-oriented, and backed by decades of research. The most proven method is Cognitive Behavioral Therapy, or CBT. It teaches you to recognize distorted thoughts-like “I’m a failure” or “Nothing will ever get better”-and replace them with more realistic ones. You don’t just talk about your past. You learn skills you can use every day. Behavioral activation is a simpler version of CBT. It’s about slowly bringing back activities you used to enjoy, even if you don’t feel like it. Go for a walk. Call a friend. Make your bed. These small actions help rewire your brain over time. Studies show they’re especially helpful in primary care settings where time with a therapist is limited. Another option is Interpersonal Therapy (IPT). It focuses on relationships. If you’re stuck in a toxic friendship, grieving a loss, or feeling isolated after a divorce, IPT helps you navigate those changes. It’s not about blaming others. It’s about understanding how your connections affect your mood-and how to improve them. For people who struggle with face-to-face sessions, computerized CBT (CCBT) is available online. You work through modules on a website or app, often with guided support. It’s convenient, especially if you live in a rural area or have mobility issues. But it’s not for everyone. You need to be motivated. And it doesn’t replace the connection you get from talking to a real person.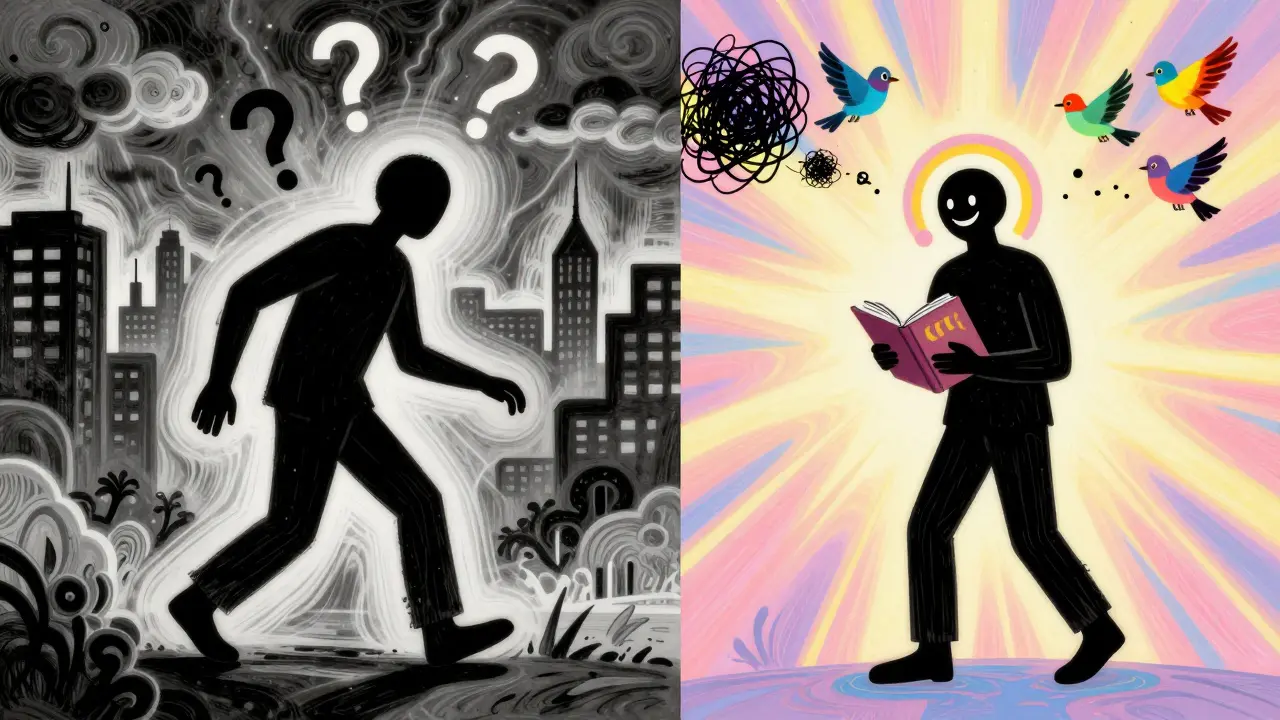
Combining Medication and Therapy: The Gold Standard
Here’s what the science says: if you have moderate to severe depression, combining antidepressants with CBT or another form of therapy gives you the best chance of recovery. A 2025 study in Nature found that people who used both treatments were significantly more likely to see their symptoms drop by more than half compared to those using just one. Why? Because medication helps balance brain chemistry, making it easier to focus and engage in therapy. Therapy helps you rebuild your thinking patterns, so you’re less likely to slip back into depression later. One person I spoke to said, “The pills helped me get out of bed. CBT helped me learn why I didn’t want to get up.” For mild depression, therapy alone often works just fine. No medication needed. In fact, guidelines from NICE and the American Academy of Family Physicians recommend starting with therapy or even just active monitoring-checking in regularly with your doctor-before jumping to pills.What Doesn’t Work (And Why)
Some people think supplements, herbal remedies, or “positive thinking” alone can cure depression. They can help as extras, but they’re not substitutes for evidence-based care. St. John’s Wort, for example, might help mild cases, but it interacts dangerously with many medications. And telling someone to “just be happy” doesn’t fix brain chemistry. Another myth: antidepressants make you “addicted.” They’re not addictive like alcohol or opioids. But stopping them suddenly can cause withdrawal symptoms-dizziness, brain zaps, nausea. That’s why you always taper off under medical supervision. And therapy isn’t a quick fix. It takes work. Most people need 12 to 20 weekly sessions. That’s a commitment. But the skills you learn? They stick with you. One Reddit user wrote: “CBT taught me tools I still use five years later.” That’s the real value.
Access and Barriers: The Real-World Challenges
Knowing what works is one thing. Getting it is another. Waiting lists for therapists can be months long, especially in rural areas. In Australia, where I live, public mental health services are stretched thin. Private therapy can cost hundreds per session. Not everyone can afford it. Telehealth has helped. Many therapists now offer video calls. Online CBT platforms like MoodGYM or This Way Up are free or low-cost. And if you’re in the U.S., the 988 Suicide & Crisis Lifeline is available 24/7. NAMI’s HelpLine (800-950-6264) also offers free support and referrals. Insurance coverage has improved. Eighty-three percent of large employers now cover mental health services. But gaps still exist. Some plans limit how many therapy sessions they pay for. Others require high copays. Always ask: “What’s covered? How many sessions? Do I need a referral?”How to Start
If you think you might have MDD, start with your doctor. They can rule out physical causes-like thyroid problems or vitamin D deficiency-that mimic depression. Then, they can refer you to a mental health professional. Ask questions:- What kind of depression do I have?
- What are my treatment options?
- What are the risks and benefits of each?
- How will we know if it’s working?
What’s Next for Treatment?
Researchers are exploring ways to personalize treatment. Some clinics now use genetic testing to predict which antidepressant might work best for you. But right now, the evidence isn’t strong enough to make it standard. Still, it’s promising. Digital tools are growing fast. Apps that track mood, guide breathing exercises, or deliver CBT lessons are becoming more sophisticated. But remember: they’re helpers, not replacements. You still need a doctor or therapist to guide you. The World Health Organization says depression will remain one of the top causes of disability worldwide through 2030. That means more research, more funding, and better access. But change takes time. Until then, the tools we have now-medication, therapy, and support-are powerful. And they work.Can antidepressants make me feel emotionally numb?
Yes, some people report feeling emotionally flat or detached while on antidepressants, especially SSRIs. This is called emotional blunting. It’s not universal, but it’s common enough that doctors know to watch for it. If it happens, your provider can adjust your dose or switch you to a different medication. Sometimes, adding therapy helps restore emotional responsiveness. Never stop medication on your own-talk to your doctor first.
How long does psychotherapy take to work?
Most people start noticing small changes after 4 to 6 weeks of weekly therapy. Significant improvement usually happens after 12 to 20 sessions. CBT and IPT are structured, so progress is often measurable. You’ll track your mood, complete homework, and practice new skills. It’s not magic-it’s practice. The longer you stick with it, the more lasting the results.
Is online therapy as effective as in-person therapy?
For many people, yes. Studies show that online CBT and video-based therapy are just as effective as face-to-face sessions for treating major depression. The key is consistency and engagement. If you’re motivated and have reliable internet, digital therapy can be a great option-especially if you live far from providers or have mobility issues. But if you need deep emotional support or have complex trauma, in-person care might be better.
What if I don’t respond to the first antidepressant I try?
That’s very common. About 30-40% of people don’t respond to their first medication. It doesn’t mean you’re broken or hopeless. It just means you need to keep trying. Doctors usually switch to a different class of antidepressant-like going from an SSRI to an SNRI-or add another medication. Sometimes, combining therapy with a different drug makes the difference. Persistence matters more than perfection.
Can I stop taking antidepressants once I feel better?
Don’t stop abruptly. Even if you feel better, stopping suddenly can cause withdrawal symptoms like dizziness, nausea, or brain zaps. Most doctors recommend staying on medication for at least 6 to 12 months after symptoms improve. For people with recurrent depression, longer-term use may be advised. Always work with your provider to taper off slowly. Therapy can help you build skills so you’re less likely to relapse after stopping.
Are there side effects I should watch for with psychotherapy?
Psychotherapy doesn’t have physical side effects like medication does. But it can bring up difficult emotions-sadness, anger, shame-as you confront painful thoughts or memories. That’s normal. A good therapist will help you process these feelings safely. If you feel worse after sessions for weeks, or if your therapist pushes you in ways that feel unsafe, it’s okay to find someone else. Therapy should feel like support, not retraumatization.


Alex Smith
January 11, 2026So let me get this straight-you’re telling me I can’t just ‘snap out of it’ but also can’t just ‘take a pill and be fine’? Wow. Groundbreaking. I feel seen.
Also, who wrote this? A psychiatrist who also moonlights as a TED Talk ghostwriter?
Sean Feng
January 12, 2026Therapy is expensive and takes too long. Pills are easier. I tried CBT once. Felt like homework. Didn’t do it.
Priscilla Kraft
January 14, 2026I’ve been in therapy for 3 years and on sertraline for 2. It’s not perfect but it’s the best thing I’ve ever done for myself 🌱
Also-emotional blunting is real. I stopped crying at movies. Then my therapist helped me switch meds. Now I cry at dog videos again. Worth it. ❤️
Vincent Clarizio
January 14, 2026Let’s be real-depression isn’t a medical condition, it’s a metaphysical crisis wrapped in neurochemical noise. You’re not broken, you’re just out of alignment with the existential fabric of a capitalist dystopia that commodifies joy and sells serotonin as a subscription service.
Antidepressants? They’re just chemical pacifiers for a society that refuses to ask why we’re all so damn miserable in the first place. Therapy helps you adapt. But adaptation isn’t healing. It’s survival with better lighting.
Sam Davies
January 16, 2026Oh look, another American mental health pamphlet dressed up as a manifesto. We’ve had CBT in the NHS since the 90s. It’s not magic, it’s just the least bad option we’ve got.
Also, ‘brain zaps’? Sounds like a bad sci-fi novel. I’d rather have a brain zap than another goddamn wellness influencer telling me to ‘manifest happiness’.
Christian Basel
January 17, 2026The pharmacokinetics of SSRIs are poorly understood at the receptor level. Most clinical trials are industry-funded and overstate efficacy. The NNT for remission is ~7. The placebo response rate is ~40%. You’re being sold a narrative wrapped in biopsychiatry jargon.
Adewumi Gbotemi
January 18, 2026In Nigeria, we don’t have pills or therapists. We have family. We have church. We have talking till your throat is sore. And it works. Not perfect. But real. This article feels like a luxury.
Michael Patterson
January 19, 2026Ive been on prozac since 2018 and i still dont know if its helping or if im just used to feeling like a zombie. also why is everyone so obsessed with cbt? i tried it and it felt like being told to smile more while your soul is rotting. therapy is for people who can afford to sit in a room and cry for $150 an hour.
Matthew Miller
January 19, 2026This is the most condescending piece of mental health propaganda I’ve read in years. You act like depression is a glitch you can patch with meds and worksheets. What about the people whose trauma is too deep for CBT? Who can’t afford meds? Who live in food deserts and sleep in cars? This isn’t a self-help blog. It’s a luxury pamphlet for people who still have access to healthcare.
Madhav Malhotra
January 21, 2026In India, we call depression 'stress' or 'too much thinking'. But I’ve seen my cousin take fluoxetine and slowly come back to life. She started painting again. We didn’t have therapy, but we had chai, silence, and no judgment. Maybe the real cure isn’t in the pill or the session-it’s in being allowed to just… be.