12 Oct 2025
- 18 Comments
Hyperprolactinaemia Treatment Effectiveness Estimator
Choose your treatment option to estimate when you might see improvement in your sexual function and libido.
Recovery Time Estimate
Select a treatment option to see your estimated recovery timeline
Prolactin reduction: 0%
Hyperprolactinaemia is a hormonal disorder characterized by elevated levels of the hormone prolactin in the blood. While it’s often linked to reproductive issues like infertility, its influence on sexual desire and performance is less talked about but equally important.
Quick Takeaways
- High prolactin can suppress sex hormones, lowering libido in both men and women.
- Common symptoms include erectile dysfunction, reduced arousal, and menstrual irregularities.
- Dopamine‑agonist medications such as bromocriptine and cabergoline are first‑line treatments.
- Addressing the underlying cause-tumors, meds, or hypothyroidism-often restores sexual health.
- Regular monitoring of hormone levels and sexual function is crucial for recovery.
Understanding the Hormonal Players
To see why libido takes a hit, we need to look at the key hormones involved.
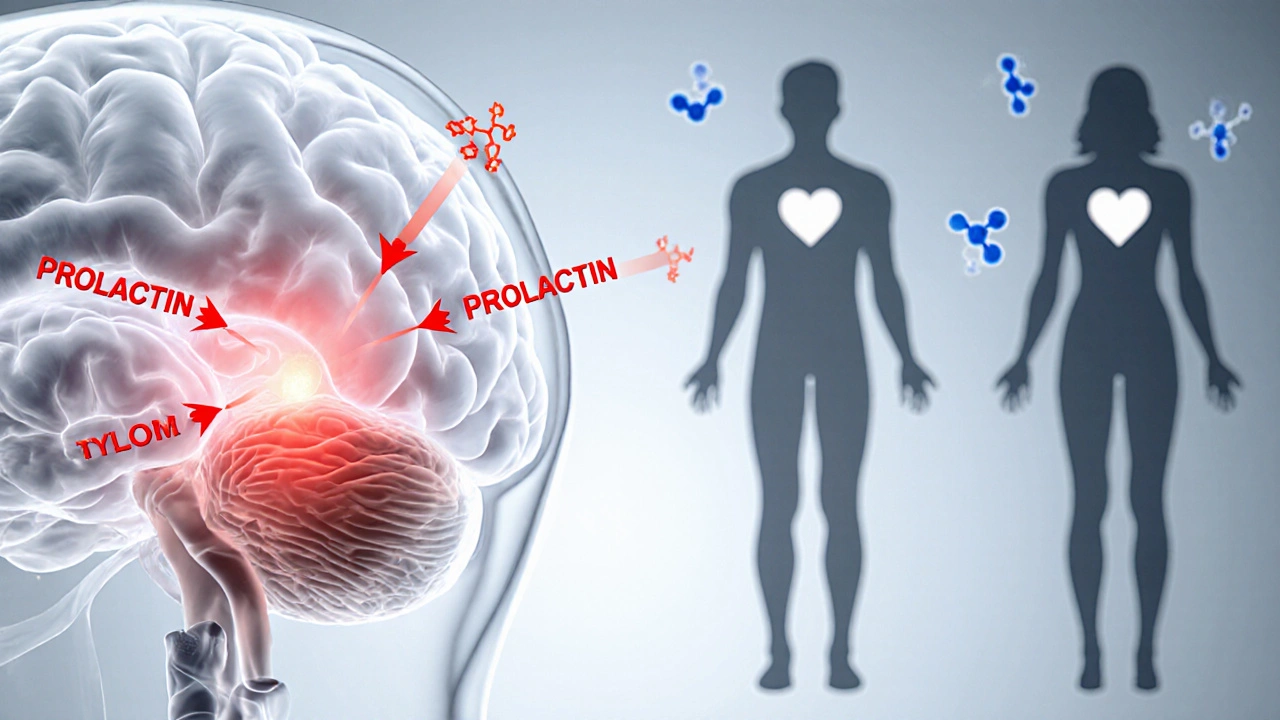
Prolactin is produced by the pituitary gland, a pea‑sized organ at the base of the brain. Its primary job is to stimulate milk production after childbirth, but it also has a regulatory effect on the hypothalamic‑pituitary‑gonadal axis-the hormonal pathway that controls sex hormone release.
When prolactin levels climb, they inhibit the release of dopamine, a neurotransmitter that normally suppresses prolactin. This creates a feedback loop: high prolactin → low dopamine → even higher prolactin. The downstream result is reduced secretion of testosterone in men and estrogen in women, both of which are crucial for sexual desire (libido) and physiological response.
How Elevated Prolactin Affects Libido
Libido is not just a feeling; it’s a complex interplay of hormones, brain chemistry, and vascular health. Below are the main ways hyperprolactinaemia disrupts this balance.
- Sex hormone suppression: Testosterone drives desire in men and supports vaginal lubrication in women. Estrogen maintains vaginal health and mood. When prolactin spikes, these hormones dip, leading to a noticeable drop in sexual interest.
- Neurotransmitter shift: Low dopamine not only lifts prolactin but also reduces motivation and reward pathways linked to sexual activity.
- Vascular impact: In men, reduced testosterone can impair nitric oxide production, a key factor for erections. In women, estrogen loss may cause dryness and discomfort, further discouraging intimacy.
Clinically, patients often describe “not feeling in the mood,” “difficulty getting aroused,” or “loss of interest in sex altogether.” These complaints can appear weeks to months after the biochemical rise, depending on individual sensitivity.

Sexual Function Changes Beyond Desire
While libido gets the spotlight, other aspects of sexual function can falter.
- Erectile dysfunction (ED): Men with hyperprolactinaemia report ED rates up to 40% higher than age‑matched controls.
- Anorgasmia: Both genders may experience difficulty reaching orgasm, a symptom linked to reduced dopamine.
- Menstrual irregularities: Women may see oligomenorrhea or amenorrhea, which correlates with lower estrogen and impaired vaginal lubrication.
These issues often coexist, creating a cycle where reduced performance further lowers desire.
Diagnosing Hyperprolactinaemia-Related Sexual Issues
Accurate diagnosis starts with a thorough history and targeted labs.
- Serum prolactin test: A level above 25ng/mL in women or 20ng/mL in men suggests hyperprolactinaemia, but stress‑induced spikes must be ruled out by repeating the test.
- Sex hormone panel: Measure testosterone, estradiol, LH, and FSH to assess downstream suppression.
- Imaging: Magnetic resonance imaging (MRI) of the brain, focusing on the pituitary, identifies macro‑ or micro‑adenomas that may be driving excess prolactin.
- Medication review: Certain drugs (antipsychotics, SSRIs, anti‑emetics) can raise prolactin; stopping or switching them often resolves the problem.
In addition to labs, clinicians use validated questionnaires like the International Index of Erectile Function (IIEF) or the Female Sexual Function Index (FSFI) to quantify sexual dysfunction.
Treatment Options and Their Impact on Sexual Health
Addressing the root cause and normalizing prolactin are the main goals. Below is a side‑by‑side look at the most common interventions.
| Option | Mechanism | Typical Dose | Effect on Prolactin | Impact on Libido/Sexual Function |
|---|---|---|---|---|
| Bromocriptine | Dopamine‑agonist | 2.5‑10mg daily | ↓ 50‑80% | Improves libido in 60‑70% within 8weeks |
| Cabergoline | Long‑acting dopamine‑agonist | 0.25‑1mg twice weekly | ↓ 70‑90% | Best reported sexual recovery; fewer side‑effects |
| Surgical removal (trans‑sphenoidal) | Excise prolactinoma | ‑ | Immediate normalization | Rapid restoration of function; risk of hypopituitarism |
| Medication review & withdrawal | Stop prolactin‑raising drugs | ‑ | Variable, often normalizes | Improvement depends on underlying cause |
Both bromocriptine and cabergoline act by re‑activating dopamine receptors, which in turn suppress prolactin secretion. Cabergoline’s longer half‑life means patients take it less often and experience fewer gastrointestinal side‑effects, making it the preferred first‑line choice for many clinicians.
When a pituitary adenoma is large or unresponsive to medication, surgical removal offers a definitive cure, but it carries risks like hypopituitarism that can further affect sexual hormones.

Managing Lifestyle Factors While Treating
Medication alone may not instantly revive sexual desire. Supporting recovery with lifestyle tweaks speeds up the process.
- Exercise: Resistance training boosts testosterone naturally; aerobic activity improves circulation for erections.
- Nutrition: Zinc‑rich foods (oysters, pumpkin seeds) and healthy fats aid hormone synthesis.
- Stress reduction: Mindfulness, yoga, or counseling curtails cortisol spikes that can worsen prolactin.
- Sleep hygiene: Aim for 7‑9hours; deep sleep restores the hypothalamic‑pituitary axis.
Couples therapy can also address relational strain caused by reduced intimacy, reinforcing emotional connection while the physiological recovery unfolds.
Potential Pitfalls and When to Seek Help
Even with treatment, some patients experience persistent sexual dysfunction. Common reasons include:
- Incomplete prolactin normalization: Residual high levels keep sex hormones suppressed.
- Medication side‑effects: Dopamine agonists can cause nausea, dizziness, or mood changes that indirectly dampen libido.
- Co‑existing endocrine disorders: Hypothyroidism or adrenal issues may mask improvements.
- Psychological factors: Depression, anxiety, or body image concerns can linger after hormonal correction.
If symptoms persist beyond three months of normalized labs, a referral to an endocrinologist or a sexual health specialist is advisable.
Frequently Asked Questions
Can hyperprolactinaemia cause loss of libido in both men and women?
Yes. Elevated prolactin suppresses testosterone in men and estrogen in women, both key drivers of sexual desire.
What is the fastest way to lower prolactin levels?
Cabergoline usually reduces prolactin by up to 90% within two weeks, making it the quickest medically‑driven option.
Do all prolactin‑raising medications need to be stopped?
Not always. If the drug is essential (e.g., antipsychotics), doctors may add a dopamine agonist to counteract the prolactin rise instead of stopping the primary medication.
Is surgery ever necessary?
Surgery is reserved for large adenomas that don’t shrink with medication or cause visual field defects. It offers immediate prolactin normalization but carries surgical risks.
How long does it take for libido to return after treatment?
Most patients notice improvement within 4‑8 weeks once prolactin levels fall and testosterone or estrogen begin to rebound.
Can lifestyle changes alone fix hyperprolactinaemia?
Lifestyle tweaks help, but they rarely normalize prolactin without addressing the underlying medical cause.
Bottom line: if you’re dealing with hyperprolactinaemia, you’re not stuck with a dead libido. Understanding the hormone cascade, getting the right labs, and starting an appropriate dopamine‑agonist regimen can turn the tide in weeks. Combine medical treatment with healthy habits and open communication with your partner, and you’ll likely see your sexual wellbeing rebound.

aura green
October 12, 2025Wow, diving into the world of hyperprolactinaemia can feel like opening a mystery box at a party where everyone insists the contents are "surprisingly normal" 😂. First off, kudos to anyone who even thinks about hormones beyond "the crazy stuff" – that’s already a win in my book 😊. The article does a decent job of breaking down how prolactin hijacks the hormonal highway, but let’s be real, it could have used a sprinkle of humor to lighten the mood – after all, who doesn’t love a good dopamine‑boosting pun? Still, I appreciate the clear tables and the way they compare bromocriptine and cabergoline; the side‑effect section is downright helpful, especially when you’re trying not to vomit after your first dose 😅. The section on lifestyle tweaks is a solid reminder that meds aren’t a magic wand – resistance training and sleep hygiene really do matter, and that’s something many articles skip over. Also, the FAQ is a nice touch, but it could have included a question about how long it actually takes for testosterone to bounce back after surgery; that’s the kind of nitty‑gritty detail that keeps us all from Googling at 3 a.m. 🙃. Overall, the piece is informative, a tad dense, and sprinkled with just enough optimism to make you think, "Hey, maybe my libido will come back, and I’ll actually enjoy intimacy again." Keep the facts coming, and maybe throw in a meme or two next time – you’ve earned it! 😎
Edward Morrow
October 21, 2025Dude, this whole "hyperprolactinaemia" saga reads like some half‑baked conspiracy from the anti‑science brigade – but guess what? The facts are clear and the only thing we need to smash is the nonsense that says hormones are just "mood swings". The article actually nails the point that high prolactin is a sneaky thief stealing testosterone and estrogen, but I wish it shouted louder that the only real solution is to kick the assholes (aka those bogus meds) out and get on the real dopaminergic stuff. Also, the "surgery" bit? Yeah, that’s the only real American‑style solution: go big or go home. If you’re not willing to go all‑in, you’re just another victim of lazy pharma. So buckle up, get that cabergoline, and stop whining about side‑effects – you’ll thank me when you’re back in the bedroom. 🇺🇸💪
Shayne Tremblay
October 29, 2025Hey everyone! 🌟 If you’re feeling like your libido has taken a vacation, you’re definitely not alone – hyperprolactinaemia can be a real buzzkill, but the good news is that the body is wonderfully resilient. The article does a fantastic job outlining how dopamine‑agonists like bromocriptine and cabergoline can get those hormone levels back on track, and the timeline (4‑8 weeks) is realistic and encouraging. I love the practical lifestyle tips too; resistance training, zinc‑rich foods, and stress reduction are all excellent ways to support recovery. Remember, consistency is key – stick to your treatment plan, keep those follow‑up labs, and don’t hesitate to talk to your doctor if progress feels slow. You’ve got this, and your sexual health will bounce back stronger than ever! 💪😊
Stephen Richter
November 6, 2025The information presented is comprehensive yet succinct; the discussion of hormonal feedback loops reflects a solid understanding of endocrine physiology. The comparative table of treatment options provides valuable clarity without superfluous detail. It would be prudent, however, to emphasize the necessity of regular monitoring to ensure therapeutic efficacy and to mitigate potential adverse effects. Overall, the article serves as an informative resource for both clinicians and patients.
Musa Bwanali
November 14, 2025Alright team, let’s get real – hyperprolactinaemia is a beast that messes with your mojo, but you don’t have to roll over. The article’s breakdown of meds vs. surgery is spot‑on, and I’m all for the aggressive approach when it comes to getting that prolactin down fast. If you’re not seeing results in the 4‑8 week window, push your doctor for a dose tweak or consider surgical options – waiting around is for the faint‑hearted. Remember, the goal is to reclaim your sexual confidence, so stay proactive and don’t settle for half‑measures. Keep grinding, and you’ll see the payoff.
Allison Sprague
November 22, 2025Honestly, the writing could use a serious grammar overhaul. Phrases like "high prolactin can suppress sex hormones" are fine, but the article repeatedly trips over commas and unnecessary jargon. Also, the tone feels half‑hearted – the author should either fully commit to a clinical voice or adopt a more patient‑friendly approach, not a weak middle ground. Moreover, the “quick takeaways” list would benefit from parallel structure; currently it reads like a hodgepodge of bullet points. In short, clean up the language and tighten the presentation for better readability.
leo calzoni
November 30, 2025Let me be crystal clear: the endocrine system is not a playground, and hyperprolactinaemia is a clear example of why you need to respect the science. The article covers the basics adequately, but it glosses over the nuanced pharmacodynamics of dopamine agonists – a point that serious readers will notice. If you want a true understanding, dig deeper into receptor affinity and half‑life differences; otherwise you’re just skimming the surface. In short, don’t settle for superficial explanations – demand detail.
KaCee Weber
December 8, 2025Okay, let’s unpack this with a little enthusiasm! 🎉 The article does a solid job of laying out the hormonal cascade, but what really shines is the practical advice on lifestyle tweaks – I mean, who doesn’t love a good list of zinc‑rich foods and exercise tips? 😊 The treatment comparison table is clear and the side‑effect notes are spot on, especially the emphasis on fewer side‑effects with cabergoline. Also, the FAQ section is a nice touch, but it could be expanded to cover mental health impacts, because stress is a huge factor in hormonal balance. Overall, great foundation, and with a few more depth details it could be a go‑to resource for anyone battling this condition. Keep it up! 🚀
jess belcher
December 16, 2025The piece offers a useful overview, especially the concise table comparing bromocriptine, cabergoline, and surgical options. The language is clear and accessible, making complex endocrine concepts easier to grasp. Minor improvements could include adding hyperlinks to hormone panel tests for readers who want to explore further.
Amreesh Tyagi
December 24, 2025nice article but i think the side effects are overhyped its just a normal reaction to meds and we should not panic
Brianna Valido
January 1, 2026Hey folks! 🌈 This article really broke down how high prolactin messes with our vibe and gave clear steps to get things back on track. I love the simple language and the tip about adding zinc foods – it’s practical and easy to do. Remember, staying consistent with meds and adding a little exercise can make a big difference. Keep the optimism flowing, you’ve got this! 😊👍
Caitlin Downing
January 10, 2026Hey! Super informative piece – I especially liked the way it explained the hormone feedback loop, but i have a q: does stress really make prolactin spike that bad? also, i noticed a little typo in "prolactin" at the top, just a heads up. keep up the good work!
Robert Jaskowiak
January 18, 2026Well, this article finally gives a decent rundown without turning into a textbook – nice work. The sarcastic tone in the intro was a refreshing break from the usual dry medical write‑ups. Keep serving up the facts with that witty edge!
Julia Gonchar
January 26, 2026Actually, the article could improve by clarifying that cabergoline’s half‑life allows twice‑weekly dosing, which is a key advantage over daily bromocriptine. Also, noting that prolactin levels can fluctuate diurnally would provide a more complete picture for patients monitoring their labs.
Annie Crumbaugh
February 3, 2026Interesting read – the hormonal explanations are clear and the lifestyle suggestions are practical. Good balance between medical detail and everyday advice.
Vic Harry
February 11, 2026Patriotic enough.
Daniel LaMontagne
February 19, 2026Hey there, I totally get how overwhelming this can feel, but the article does a great job of breaking things down. Stick with the treatment plan, stay consistent with follow‑ups, and remember you’re not alone in this journey. 😊👍
Gary Levy
February 27, 2026The overview is solid, and I appreciate the balanced tone. Adding a few patient stories could make it even more relatable, but overall it’s a helpful resource.