15 Dec 2025
- 10 Comments
When you pick up a prescription, you might not realize that the pill in your hand isn’t always the one your doctor wrote on the slip. In most states, your pharmacist can swap a brand-name drug for a cheaper generic version - unless your doctor says no. But here’s the catch: pharmacy substitution laws vary wildly from state to state. What’s allowed in California might be illegal in Oklahoma. And if you’re switching to a biosimilar for a biologic drug like Humira or Enbrel, the rules get even more complicated.
What Exactly Is Pharmacy Substitution?
Pharmacy substitution means a pharmacist gives you a different drug than what’s written on the prescription - usually a generic version. Generics contain the same active ingredient, dose, and route of delivery as the brand-name drug. They’re not knockoffs. They’re FDA-approved copies that cost 80-85% less. For example, a 30-day supply of brand-name Lipitor might cost $300, while atorvastatin (the generic) runs about $10. But here’s the thing: just because a generic is cheaper doesn’t mean it’s automatically substituted. Every state has its own rules. Some require pharmacists to swap unless told otherwise. Others say substitution is optional. And in a few, you have to give explicit permission before they switch anything.State Laws Fall Into Three Categories
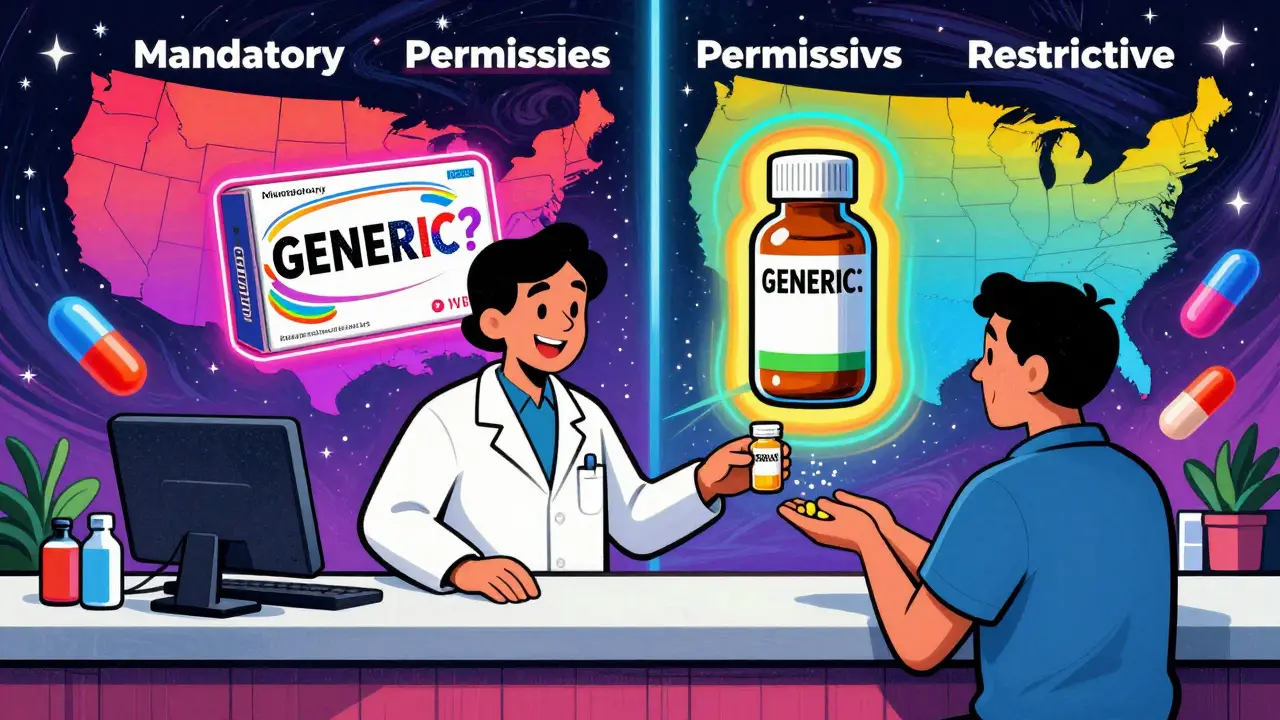
There’s no national standard. Instead, states have grouped their laws into three main types:- Mandatory substitution: Pharmacists must substitute unless the prescriber writes “dispense as written.” This applies in 19 states, including New York, Texas, and California.
- Permissive substitution: Pharmacists can substitute, but aren’t required to. This is the case in 31 states plus Washington, D.C. They’ll often do it anyway - because it saves money and the insurer usually pays more for the generic.
- Restrictive substitution: Some states block substitution for certain drugs, especially those with narrow therapeutic indexes (NTI). These are meds where even tiny differences in formulation can cause harm. Think warfarin (blood thinner), phenytoin (seizure drug), or levothyroxine (thyroid). States like Kentucky and Hawaii maintain official lists of these drugs and prohibit substitution without explicit approval.
Do You Need to Give Consent?
In 7 states and D.C., pharmacists can’t switch your medication without your direct, verbal or written consent. That means they have to ask you: “Do you want this generic instead?” In 31 states and D.C., they only need to notify you after the fact - usually by putting a sticker on the bottle or adding a note to your receipt. You might not even notice the change until you check the label later. And in 19 states? No notification or consent is required at all. You could walk in for your brand-name drug and walk out with a generic - and never know unless you compare the pills. This matters. If you’ve had bad reactions to a specific generic brand before, or if you’re on multiple meds that interact in complex ways, you deserve to know what’s in your hand.
Biosimilars Are a Whole Different Ballgame
If you’re taking a biologic drug - like Humira, Enbrel, or Remicade - substitution gets even trickier. These aren’t simple chemical copies. They’re made from living cells, so they’re harder to replicate exactly. The FDA calls them “biosimilars.” But here’s the key: not all biosimilars are created equal. Only 10 out of 38 approved biosimilars have been designated as “interchangeable” by the FDA as of late 2023. That means they’ve met extra standards proving they can be swapped without increasing risk. Even then, 45 states (90%) impose extra rules on biosimilar substitution that don’t apply to regular generics. Most common? You need to be notified - and sometimes your doctor does too. In 37 states, pharmacists must tell your prescriber within 7 days after swapping a biosimilar. In 12 states, they need your doctor’s permission before substituting at all. And in 15 states, they can’t substitute if the biosimilar costs more than the original - even if your insurance covers it. States like Florida, Georgia, and Illinois require dual notification: both you and your doctor must be informed within 24-72 hours. Meanwhile, Alabama and Mississippi have almost no extra rules beyond basic recordkeeping.What Can You Do as a Patient?
You have rights - even if the law doesn’t always make them obvious.- Ask: When you get your prescription filled, ask: “Was this substituted?” Check the label. Generic names are often printed in smaller font.
- Refuse: You can say no to substitution in every state. Pharmacists can’t force you to take a generic, even if it’s cheaper.
- Check your doctor’s note: If your doctor wrote “dispense as written” or “do not substitute,” that overrides state law. It’s legally binding.
- Call your state board of pharmacy: Each state has one. They can tell you exactly what’s allowed. A quick Google search for “[Your State] board of pharmacy substitution laws” will get you there.
- Keep a list: If you’re on NTI drugs or biologics, write down every medication you take - brand and generic names - and share it with every pharmacist. It helps avoid dangerous mix-ups.
What Can Prescribers Do?
Doctors can block substitution by writing “dispense as written” on the prescription. But in 28 states, they also have to explain why - like “patient had adverse reaction to generic” or “therapeutic instability.” That adds paperwork. Some prescribers avoid the hassle and just write the brand name. That’s fine - but it costs more. And if you’re paying out of pocket, you’re paying the difference. If you’re a provider, know your state’s rules. If you’re prescribing warfarin, phenytoin, or levothyroxine, always check if your state restricts substitution. And if you’re prescribing a biologic, understand whether the generic version is even interchangeable - and whether your state requires notification.
Why This Matters for Your Health
Generic substitution saves the U.S. healthcare system $313 billion a year. That’s huge. But cost savings shouldn’t come at the cost of safety. A 2018 study found that states with restrictions on substituting NTI drugs saw 18% fewer adverse events. That’s not a small number. It means real people avoided hospitalizations, bleeding episodes, or seizures because their meds didn’t change unexpectedly. For biologics, the stakes are even higher. A patient on a biosimilar might have a different immune response than on the original. If you’re on one for rheumatoid arthritis or Crohn’s disease, a switch could trigger a flare-up. That’s why notification matters. You need to know if your treatment changed - so you can watch for side effects and tell your doctor.What’s Changing in 2025?
More biosimilars are getting interchangeable status. By 2030, they could make up 70% of the biologics market. That means substitution will become more common - and state laws will need to catch up. California and New York updated their laws in early 2023 to strengthen patient notification for biosimilars. Other states are following. The National Association of Boards of Pharmacy is pushing for standardized rules across states - especially around documentation and timing of notifications. But until then, you’re stuck with a patchwork system. Your rules depend on where you live - and where your pharmacy is.Bottom Line: Know Your State, Know Your Rights
You don’t need to be a pharmacist to navigate substitution laws. But you do need to be informed. - If you’re on a high-risk medication, assume substitution is possible - and ask. - If you’ve had a bad experience with a generic before, tell your doctor and pharmacist - and ask them to write “dispense as written.” - If you’re switching states, check the rules. What worked in Florida might not fly in Pennsylvania. - If you’re paying cash, ask if the generic is cheaper - and if it’s the same thing. Pharmacy substitution isn’t good or bad. It’s a tool. Used right, it saves money without sacrificing care. Used wrong, it can cause harm. The difference? Awareness.Can my pharmacist substitute my brand-name drug without telling me?
Yes - in 19 states, pharmacists can substitute generic drugs without notifying you. In 31 states and D.C., they must notify you after the fact, usually on the label or receipt. Only 7 states and D.C. require your explicit consent before substitution. Always check your prescription label for the generic name - it’s often printed in smaller text.
Can I refuse a generic substitution?
Yes. You have the right to refuse a generic or biosimilar substitution in every state. You can say “no” at the pharmacy counter. If you’re on a medication with a narrow therapeutic index - like warfarin or thyroid hormone - it’s especially important to speak up. You can also ask your doctor to write “dispense as written” on your prescription to prevent substitution entirely.
What’s the difference between a generic and a biosimilar?
Generics are chemically identical copies of small-molecule drugs, like statins or antibiotics. Biosimilars are copies of complex biologic drugs - like Humira or Enbrel - made from living cells. They’re not exact copies, so they must go through stricter FDA review. Only 10 of the 38 approved biosimilars have received “interchangeable” status, meaning they can be substituted like generics. The rest require special rules under state law.
Which drugs can’t be substituted at all?
Drugs with narrow therapeutic indexes (NTI) are often restricted. These include warfarin (blood thinner), phenytoin (seizure control), levothyroxine (thyroid hormone), and lithium (bipolar disorder). In states like Kentucky and Hawaii, substitution of these drugs requires explicit approval from both the prescriber and patient. Even if your state allows substitution, your pharmacist may still refuse to swap these due to safety risks.
How do I find out my state’s substitution rules?
Visit your state’s Board of Pharmacy website. Search for “[Your State] Board of Pharmacy substitution laws.” Most have downloadable guides or FAQs. You can also call them directly - they’re required to answer public questions. For biosimilars, check the National Association of Boards of Pharmacy’s model legislation page - 22 states have adopted parts of it since 2020.

Josias Ariel Mahlangu
December 16, 2025People don’t realize how dangerous this is. I’ve seen patients on warfarin switch generics and end up in the ER. It’s not about cost-it’s about control. Pharmacists shouldn’t be making therapeutic decisions. If your doctor prescribes a specific brand, that’s because they know your body. Let them decide, not some guy behind a counter trying to hit a quota.
And don’t get me started on biosimilars. These aren’t generics. They’re biologics with subtle differences that can trigger immune responses. No one’s tracking long-term effects. We’re basically guinea pigs for corporate savings.
States need to mandate consent. Full stop. No exceptions. This isn’t choosing between Coke and Pepsi-it’s your life.
Cassandra Collins
December 16, 2025ok so here’s the real tea 🫖 the FDA is in bed with big pharma and they’re letting pharmacists swap drugs to make you dependent on cheaper versions that dont work right? and then they dont even tell you??
i had a friend take a generic for her seizure med and she had a full-on convulsion 3 days later. hospital. brain scan. everything. they said it was "probably the switch" but the pharmacist just shrugged.
theyre hiding this from you. they dont want you to know you’re being experimented on. call your state rep. now. #pharmacracy
Joanna Ebizie
December 17, 2025lol y’all act like this is news. every time i pick up my thyroid med, i check the label like a hawk. if it’s not the same little blue pill with the weird crack on the side? i walk back in and demand the original.
they think i don’t know the difference? honey, i’ve been on levothyroxine since 2012. i know my body. if the generic makes me jittery or tired? it’s not me-it’s the filler. and i ain’t taking it.
just say no. and if they give you attitude? tell ‘em you’re filing a complaint with the board. they hate that.
Elizabeth Bauman
December 18, 2025As an American citizen who pays taxes and follows the law, I find this entire system unacceptable. We have the most advanced medical system in the world, yet we allow foreign-owned pharmacy chains to swap life-saving medications without consent? This is a betrayal of public trust.
States like California and New York are leading the charge, but the rest? They’re letting corporate greed override patient safety. The FDA should be enforcing national standards-not letting 50 different states play Russian roulette with people’s health.
And biosimilars? That’s not innovation. That’s pharmaceutical colonialism. We’re exporting our medical risks to the rest of the world while pretending it’s cost-saving. Shameful.
Dylan Smith
December 18, 2025I didn’t even know this was a thing until last month when my blood pressure med changed and I felt like I was floating. I went back to the pharmacy and asked what happened. They said it was generic. I didn’t even know I was on brand until then.
Now I always ask. Always check the label. I keep a list of every med I take, brand and generic, in my phone. I showed my doctor and he was surprised I didn’t know sooner. Turns out he didn’t write "dispense as written" because he assumed the pharmacy would just do what’s cheapest.
So now I’m the one pushing back. And I’m telling everyone I know to do the same. It’s not complicated. Just ask. Always.
Mike Smith
December 20, 2025Thank you for this thorough and essential guide. The distinction between mandatory, permissive, and restrictive substitution laws is critical for patients to understand. Many assume that all generics are interchangeable and safe, but that assumption can lead to serious consequences, particularly with narrow therapeutic index medications.
I encourage every patient to request a printed copy of their pharmacy’s substitution policy. Most states require pharmacies to provide this upon request. Additionally, patients should maintain a personal medication log that includes both brand and generic names, manufacturer, and lot number-this information can be lifesaving in the event of an adverse reaction.
Remember: your health is not a commodity. You have the right to be informed, to refuse, and to advocate for yourself. Pharmacists are trained professionals, but they are not your prescriber. That role remains with your physician.
Knowledge is power-and in this case, it’s also protection.
Ron Williams
December 20, 2025Been in the US for 12 years and never knew this. I’m from a country where the pharmacist just gives you what’s on the script, no questions. Here, it’s like a whole legal drama every time you pick up meds.
My aunt’s on warfarin. She’s terrified of switching. We called her pharmacy, asked them point-blank if they substitute, and they said yes unless the doctor says no. She’s now asking her doc to write "dispense as written" on everything. Smart move.
Also, just checked my last prescription-generic was on the bottle. I didn’t notice. I’m gonna start checking the font size now. Thanks for the heads-up.
Kitty Price
December 21, 2025Just checked my last prescription and it was switched 😳
Thank you for this. I’m printing out the state rules for my state and taping them to my fridge. I’m also asking my doctor to write "dispense as written" on all my biologics now. I’ve been on Humira for 5 years and I don’t want any surprises.
Also-why do generics always come in different colors? It’s so confusing. I need a pill identifier app now 🤭
Aditya Kumar
December 22, 2025whatever
Colleen Bigelow
December 24, 2025Let me guess-this whole "generic substitution" thing is just a Trojan horse for the globalist pharmaceutical cartel to phase out American-made drugs and replace them with Chinese-manufactured generics that contain undisclosed fillers and heavy metals.
They don’t want you to know that the FDA’s "approval" process is a joke. The same companies that make the brand drugs own the generics. Same factories. Same owners. Same lies.
And biosimilars? That’s the next phase. They’re not even real drugs-they’re lab-grown imitations with immune-triggering contaminants. The CDC’s been hiding the spike in autoimmune flare-ups since 2021. You think that’s coincidence?
They’re testing population control through medication manipulation. Wake up. Demand transparency. Or keep swallowing the lies.