17 Dec 2025
- 0 Comments
When you're managing heart failure or atrial fibrillation, digoxin can be a lifeline. But it's also one of the most dangerous drugs if you don't know what to watch for. This isn't just about taking a pill every morning-it's about understanding how everything else in your life can turn a helpful medicine into a serious threat.
Why Digoxin Is Different
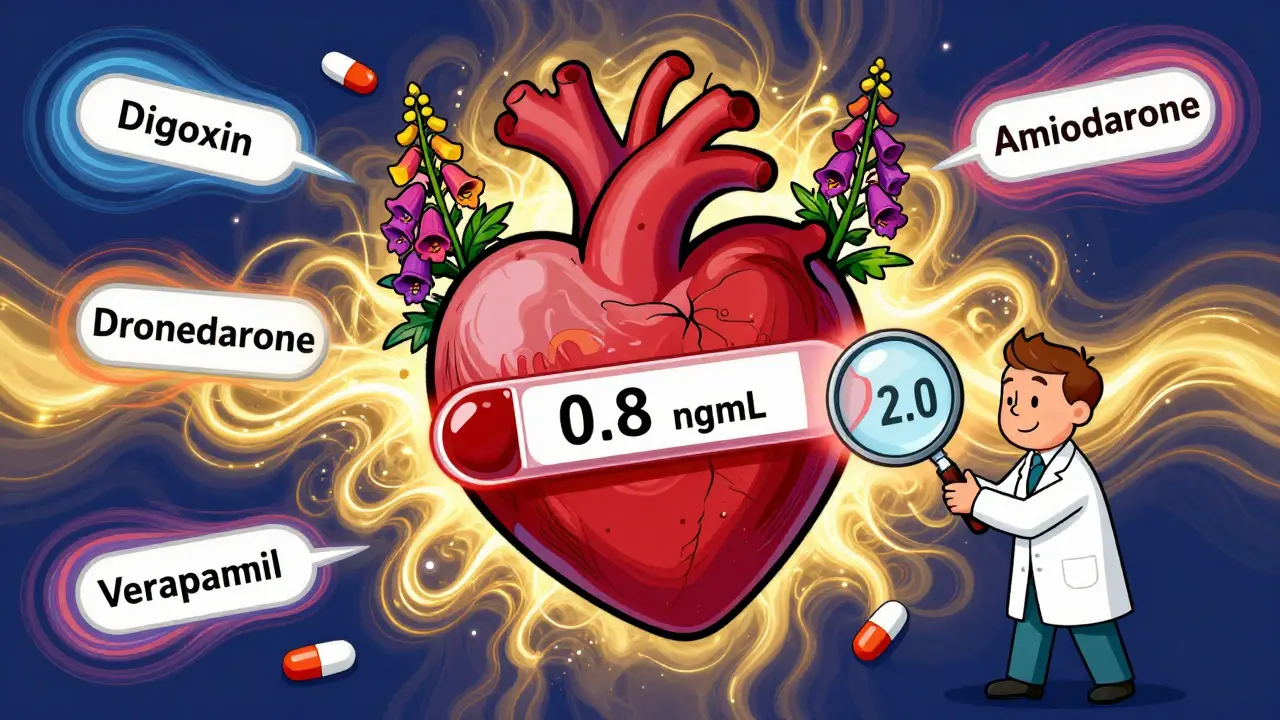
Digoxin doesn't work like most heart meds. It comes from the foxglove plant, and it's been used since the 1930s. Unlike newer drugs that target blood pressure or fluid buildup, digoxin strengthens your heart's squeeze. That sounds good, right? But here's the catch: the difference between the right dose and a dangerous one is tiny. Doctors aim for blood levels between 0.5 and 0.9 ng/mL. Go over 2.0, and you're in danger zone.
That narrow window is why so many patients end up in the ER. According to the DIG trial, even people on "normal" doses can have toxicity if they have kidney problems, are over 65, weigh less than 60 kg, or have low potassium. And those aren't rare cases. About 1 in 25 people on digoxin will have some sign of toxicity. For older adults, it's even higher.
Top 5 Drug Interactions That Can Kill You
Most people know to tell their doctor about new prescriptions. But many don't realize that even common meds can turn digoxin into poison.
- Dronedarone (for atrial fibrillation): This drug can push digoxin levels up by over 50%. In the PALLAS trial, patients on both drugs had more than double the risk of sudden death. If you're on both, your digoxin dose must be cut in half-and you need weekly blood tests for at least two weeks.
- Verapamil and Diltiazem (for high blood pressure or chest pain): These calcium channel blockers slow how fast your body clears digoxin. Levels can jump 30-50%. The result? Heart rates dropping below 40 bpm. That's not just slow-it's life-threatening.
- Amiodarone (another rhythm drug): One patient on Reddit shared how their digoxin level shot from 0.8 to 1.9 ng/mL after starting amiodarone. They got nauseous, saw halos around lights, and almost needed a pacemaker. This happens because amiodarone blocks the pump that removes digoxin from your body.
- Quinidine: This older antiarrhythmic can make digoxin levels double. It's rarely used now, but if you're on it, your doctor must reduce your digoxin by 50% immediately.
- Erythromycin and Tetracycline (antibiotics): These don't just treat infections-they change the bacteria in your gut that normally break down digoxin. That means more of the drug stays in your system. Even a 10-day course can push you into toxicity.
The Sneaky Interactions You Might Not Think About
It's not just prescription drugs. Everyday things can mess with digoxin too.
- Black licorice: Yes, really. The compound glycyrrhizin in licorice pulls potassium out of your body. Low potassium + digoxin = a recipe for dangerous heart rhythms. Even one piece a day can be risky.
- High-fiber foods: Oatmeal, bran cereal, psyllium supplements-these can reduce digoxin absorption by up to 40%. One patient found their levels were stable only after switching from taking digoxin with breakfast to taking it two hours before.
- Antacids: Aluminum and magnesium in over-the-counter heartburn meds can block digoxin from being absorbed. The Mayo Clinic found that 22% of digoxin-related ER visits were linked to these common pills.
- St. John’s Wort: This herbal supplement for depression actually makes your body get rid of digoxin faster. Levels can drop by 25%, meaning your heart isn't getting the benefit anymore.
- Hawthorn: Often sold as a natural heart remedy, hawthorn can add to digoxin's effect on the heart's electrical system, increasing the risk of dangerous rhythms.

What Your Doctor Should Be Checking
Monitoring isn't optional. It's mandatory. Here's what needs to happen:
- Digoxin blood levels: At least every 3-6 months if you're stable. But if you start a new drug, get tested weekly for two weeks. The new ACC risk score says if you're over 75, have low potassium, or take verapamil, you need weekly checks.
- Potassium levels: Check monthly. If your potassium is below 3.5 mmol/L, your risk of toxicity jumps. Diuretics like furosemide or hydrochlorothiazide are the usual culprits. Your doctor may need to switch you to a potassium-sparing diuretic like spironolactone.
- Kidney function: Digoxin leaves your body through your kidneys. If your creatinine clearance drops below 50 mL/min, your dose must be lowered. For those under 15 mL/min, many guidelines now say avoid digoxin entirely.
- Heart rate and rhythm: If your pulse drops below 50 bpm, or you feel dizzy, faint, or notice skipped beats-call your doctor. Don't wait.
What You Can Do Right Now
You don't need to be a medical expert to protect yourself. Here’s your action list:
- Take digoxin at the same time every day, preferably on an empty stomach or two hours before or after meals.
- Avoid black licorice completely. No exceptions.
- Never start a new medication, supplement, or OTC pill without checking with your pharmacist or doctor. Even something as simple as a cold medicine can interact.
- Keep a written list of every drug, herb, and supplement you take-and bring it to every appointment.
- Know your numbers: Ask for your last digoxin level and potassium result. Write them down. If you don't know them, you can't manage your risk.
- Watch for warning signs: Nausea, vomiting, loss of appetite, blurry vision, yellow or green halos around lights, confusion, or an unusually slow heartbeat. These aren't "just side effects"-they're red flags.
Why Digoxin Is Still Used (Even With All the Risks)
It's true: fewer people are on digoxin than 15 years ago. Prescriptions in the U.S. dropped 38% since 2010. But it's still in use for a reason. For patients with persistent heart failure symptoms-even after taking the best drugs like ACE inhibitors, beta-blockers, and diuretics-digoxin can improve quality of life. It reduces hospital visits. It helps people breathe easier.
And it's cheap. A month's supply costs $4 to $6. Compare that to newer drugs like sacubitril/valsartan or SGLT2 inhibitors, which can cost over $500 a month. For many, especially older adults on fixed incomes, digoxin is the only realistic option.
It's not about avoiding digoxin. It's about using it smartly. The 2023 ACC Expert Consensus says it still has a place-if you're monitored closely, know your risks, and avoid the big interaction traps.
What's Coming Next
There's hope on the horizon. The DIG-FAST trial is testing a new extended-release version of digoxin that causes fewer spikes and drops in blood levels. Early results suggest it could cut interaction risks by 30%. If it works, it could bring digoxin back into safer use for more people.
For now, the message is clear: digoxin isn't going away. But it demands respect. It's not a drug you can take on autopilot. You need to be an active participant in your care. Ask questions. Track your symptoms. Know your numbers. Because when it comes to digoxin, the smallest mistake can have the biggest consequences.
Can I take digoxin with my morning oatmeal?
No, not at the same time. High-fiber foods like oatmeal, bran, and psyllium can reduce digoxin absorption by up to 40%. Take digoxin at least two hours before eating breakfast to make sure your body gets the full dose.
What should I do if I miss a dose of digoxin?
If you miss a dose and remember within 12 hours, take it right away. If it's been more than 12 hours, skip the missed dose and take your next dose at the regular time. Never double up. Digoxin builds up in your system, and taking too much can lead to serious toxicity.
Is digoxin safe if I have kidney problems?
It can be, but only with strict monitoring. If your kidney function is reduced (creatinine clearance below 50 mL/min), your doctor must lower your dose. If your clearance is below 15 mL/min, most guidelines recommend avoiding digoxin altogether because your body can't clear it safely.
Can I drink alcohol while taking digoxin?
Moderate alcohol is usually okay, but heavy drinking can worsen heart rhythm problems and lower potassium levels-both of which increase digoxin toxicity risk. If you drink regularly, talk to your doctor about how much is safe for you.
Why do I need to check my potassium so often?
Low potassium makes digoxin much more toxic-even if your digoxin level is in the "normal" range. Diuretics, vomiting, diarrhea, or even sweating too much can drop your potassium. Checking it monthly helps catch this before it causes dangerous heart rhythms.
Are there any natural alternatives to digoxin?
There are no proven natural alternatives that work the same way as digoxin for heart failure or atrial fibrillation. Supplements like hawthorn or CoQ10 may support heart health, but they don't replace digoxin's specific effect on heart muscle contraction. Never stop digoxin for an herbal remedy without talking to your doctor.
What should I do if I start feeling nauseous or see halos around lights?
Call your doctor immediately. These are classic signs of digoxin toxicity. Don't wait to see if it passes. You may need an emergency blood test and possibly an antidote called digoxin-specific antibody fragments (Digibind). Delaying care can be life-threatening.
Can I take digoxin before a heart procedure like cardioversion?
Usually not. Your doctor will likely tell you to reduce or skip your digoxin dose 1-2 days before cardioversion. High digoxin levels can make the heart more sensitive to electrical shocks and increase the risk of dangerous rhythms during the procedure.