19 Jan 2026
- 11 Comments
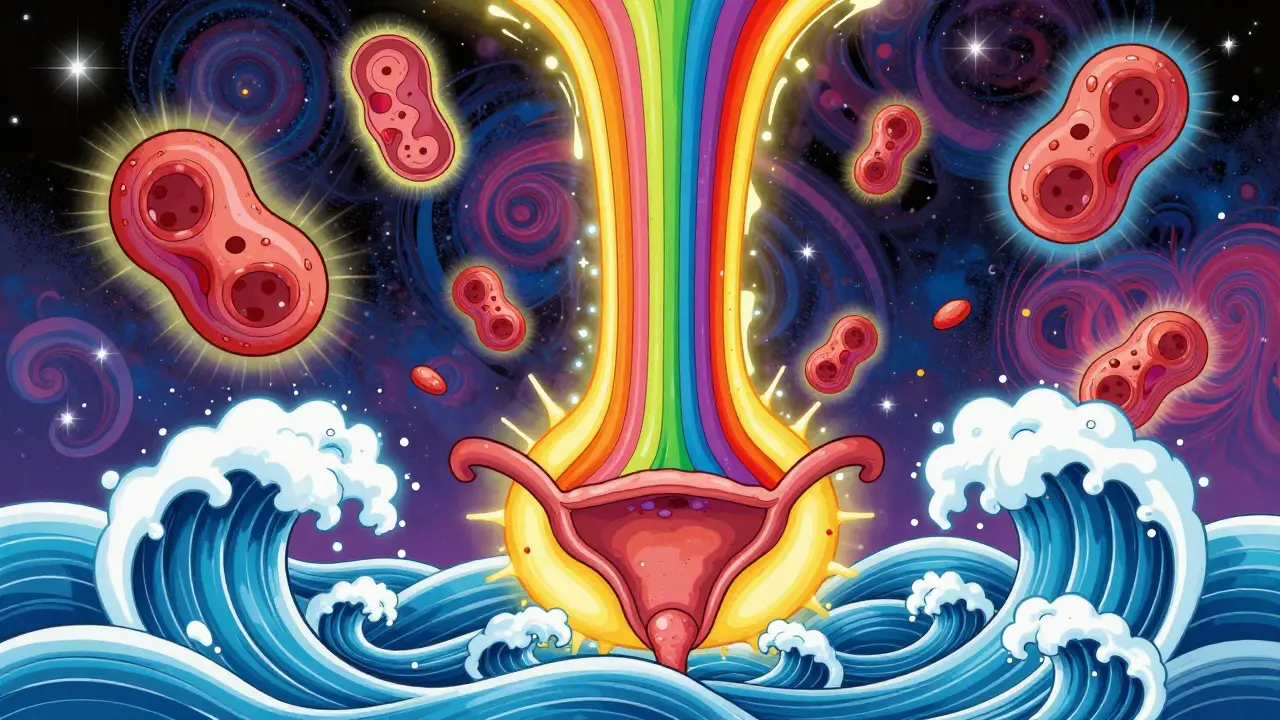
Ulcerative colitis isn’t just frequent diarrhea or occasional stomach cramps. It’s a chronic, unpredictable condition where your immune system turns on your own colon, causing open sores, constant inflammation, and a life that can feel out of control. Unlike a stomach bug that fades in a few days, ulcerative colitis (UC) sticks around - sometimes quiet, sometimes raging - and it doesn’t care about your plans. But here’s the truth: most people with UC don’t live in constant pain. With the right strategy, long periods of remission aren’t just possible - they’re common.
What Exactly Happens in Your Colon With Ulcerative Colitis?
Ulcerative colitis attacks the innermost lining of your large intestine - your colon and rectum. It doesn’t skip around like Crohn’s disease. Instead, it starts in the rectum and creeps upward, always in a continuous line. No healthy patches in between. Just inflamed, ulcerated tissue from the bottom up.
The inflammation doesn’t just make you feel sick. It breaks down the protective barrier of your colon. Blood, mucus, and pus leak into your stool. Your colon walls swell, losing their ability to hold water - which is why diarrhea becomes constant and urgent. You might feel like you’re always on the way to the bathroom, even when you’ve just gone. That’s tenesmus - the painful, false urge to pass stool. It’s not just inconvenient. It’s exhausting.
There are five main types of UC, based on how far the inflammation spreads:
- Ulcerative proctitis: Only the rectum is affected. Symptoms are often limited to rectal bleeding and mild discomfort.
- Proctosigmoiditis: Involves the rectum and lower sigmoid colon. More frequent bloody stools and cramping.
- Left-sided colitis: Extends from the rectum to the splenic flexure (near the spleen). Causes left-sided abdominal pain, weight loss, and more severe diarrhea.
- Pancolitis: Affects the entire colon. This is the most serious form - you might have more than 10 bloody bowel movements a day, severe fatigue, fever, and significant weight loss.
- Rectal-sparing UC: Rare. The rectum stays healthy, but inflammation hits the rest of the colon.
It’s not just your gut. About one in three people with UC develop problems outside the digestive tract - joint pain, red or itchy eyes, skin rashes, or liver issues. These are called extraintestinal manifestations. They’re not random. They’re your immune system misfiring, attacking other parts of your body.
What Causes Ulcerative Colitis? (And What Doesn’t)
Here’s the frustrating part: no one knows exactly what triggers UC. It’s not your fault. You didn’t eat too much junk food. You didn’t stress yourself into it. Stress and diet don’t cause UC - but they can absolutely make it worse.
What we do know is that UC is an autoimmune condition. Your immune system, which is supposed to protect you from germs, mistakenly sees the lining of your colon as a threat. It sends inflammatory cells to attack. Over time, this constant attack wears away the tissue, creating ulcers.
Some people are more at risk:
- People of Caucasian or Ashkenazi Jewish descent
- Those with a close family member who has UC or another autoimmune disease like psoriasis or rheumatoid arthritis
- People between the ages of 15-30 or 50-70 - these are the two main spikes in diagnosis
It’s not contagious. It’s not caused by a virus or bacteria you caught. And it’s not something you can outgrow. Once you have it, you’ll need to manage it - but you don’t have to let it define you.
How Do You Know If It’s UC and Not Something Else?
Many people mistake UC for irritable bowel syndrome (IBS), food poisoning, or even a bad case of the flu. But there are key differences.
IBS causes cramping, bloating, and changes in bowel habits - but no bleeding, no ulcers, no inflammation. UC does. If you’re seeing blood in your stool regularly, especially with abdominal pain and urgency, that’s not normal. It’s a red flag.
Doctors diagnose UC through a combination of:
- Medical history and symptom review
- Stool tests to rule out infections
- Blood tests to check for anemia or inflammation markers
- Colonoscopy - the gold standard. A thin camera is inserted into your colon to look for ulcers and take tissue samples
During a colonoscopy, your doctor can see exactly how far the inflammation has spread and how severe it is. This helps determine your UC type and guides treatment. It’s also how they screen for colon cancer - a risk that increases the longer you’ve had pancolitis.

How to Get Into Remission - The Real Game Plan
Remission doesn’t mean you’re cured. It means your symptoms are gone, your colon is healing, and your immune system has stopped attacking. And yes, it’s achievable - for most people.
Treatment follows a step-by-step approach:
- Mild to moderate UC: Start with 5-aminosalicylates (5-ASAs). These include mesalamine (Asacol, Lialda), sulfasalazine, or balsalazide. They’re anti-inflammatory drugs that target the colon directly. Many people stay in remission for years on these alone.
- More severe or unresponsive UC: Add immunomodulators like azathioprine or 6-mercaptopurine. These suppress your immune system more broadly to calm the inflammation.
- Moderate to severe UC that won’t respond: Biologics. These are targeted drugs like infliximab (Remicade), adalimumab (Humira), or vedolizumab (Entyvio). They block specific proteins involved in inflammation. Many patients see dramatic improvement - sometimes within weeks.
- Severe, life-threatening flares or cancer risk: Colectomy - surgical removal of the colon. This is the only true cure for UC. After surgery, you’ll need an ileostomy or a J-pouch (a surgically created internal pouch from the small intestine). Most people report a huge improvement in quality of life after surgery, even if it sounds drastic.
It’s not one-size-fits-all. What works for one person might not work for another. That’s why tracking your symptoms and working closely with a gastroenterologist matters.
What You Can Do Every Day to Stay in Remission
Medication is the backbone - but daily habits are the foundation.
Diet isn’t the cause, but it’s a trigger. There’s no universal UC diet. But many people find that during flares, certain foods make symptoms worse:
- High-fiber foods like raw vegetables, nuts, and seeds
- Dairy (if you’re lactose intolerant)
- Spicy foods
- Caffeine and alcohol
- Artificial sweeteners like sorbitol
Keep a food journal. Note what you eat and how you feel 24 hours later. Over time, you’ll spot your personal triggers. During remission, you might tolerate more foods. Don’t restrict yourself unnecessarily - nutrition matters.
Stress doesn’t cause UC, but it can ignite a flare. When your body is under stress, your immune system gets more active. That’s bad news if you already have an overactive immune system attacking your colon.
Try:
- Regular exercise - even walking 20 minutes a day helps
- Mindfulness or meditation apps
- Therapy or support groups
- Good sleep habits
Don’t skip your colonoscopies. If you’ve had UC for 8-10 years, especially with pancolitis, your risk of colon cancer increases. Regular screenings catch precancerous changes early. It’s not a scary procedure - it’s your best insurance against serious complications.
What to Expect Long-Term
UC is lifelong. But it doesn’t have to be debilitating. Studies show that 70-80% of people with UC can achieve and maintain remission with proper treatment. Many work full-time, travel, raise families, and live full lives.
The key is consistency. Taking your meds even when you feel fine. Seeing your doctor regularly. Listening to your body. Flare-ups will happen - but they don’t have to last for weeks. Early intervention can cut them short.
And remember: you’re not alone. Millions of people manage UC every day. The goal isn’t perfection. It’s control. It’s knowing you can wake up without dread. It’s having the freedom to leave the house without planning your route around every bathroom.
Remission isn’t a fantasy. It’s a realistic outcome - if you’re willing to partner with your care team and take charge of your daily habits.
Frequently Asked Questions
Can ulcerative colitis be cured?
The only true cure is removal of the colon through surgery. But for most people, UC is managed - not cured - with medication. Long-term remission is common, and many live symptom-free for years without needing surgery.
Does stress cause ulcerative colitis?
No. Stress doesn’t cause ulcerative colitis. But it can trigger flare-ups. When you’re stressed, your immune system reacts more strongly - and if you already have an autoimmune condition, that can reignite inflammation in your colon.
Can I eat normally with ulcerative colitis?
Yes - but not always. During flares, high-fiber, spicy, or dairy-heavy foods may worsen symptoms. In remission, many people tolerate a wider variety. There’s no universal UC diet. Keep a food diary to find your personal triggers and adjust accordingly.
Is ulcerative colitis the same as Crohn’s disease?
No. Both are types of inflammatory bowel disease, but they’re different. UC only affects the inner lining of the colon and rectum, in a continuous pattern. Crohn’s can affect any part of the digestive tract, including the mouth and anus, and involves deeper layers of tissue with patchy, skipped areas of inflammation.
Will I need surgery?
Not everyone does. Surgery is usually considered if medications fail, if you have severe complications like heavy bleeding or perforation, or if cancer risk becomes too high. Many people manage UC for decades without surgery. But for those who do have it, quality of life often improves significantly afterward.
Can ulcerative colitis lead to colon cancer?
Yes, especially if you’ve had pancolitis for more than 8-10 years. That’s why regular colonoscopies are critical. Screening catches precancerous changes early, and removing them prevents cancer from developing. Your doctor will recommend how often you need them based on your disease extent and duration.
Next Steps
If you’ve been diagnosed with UC, start by finding a gastroenterologist who specializes in inflammatory bowel disease. Don’t settle for a general practitioner if your symptoms aren’t improving. UC requires expert care.
Start a symptom journal. Track bowel movements, pain levels, diet, stress, and sleep. Bring it to your next appointment. It’s the fastest way to find patterns and adjust treatment.
If you’re in remission, don’t stop your meds. Most flares happen because people feel better and quit their treatment too soon. Stay consistent. Your colon is still healing - even if you don’t feel it.
And if you’re newly diagnosed - breathe. You’re not broken. You’re not alone. UC is a challenge, but it’s not a sentence. With the right plan, you can live well - for decades.

Courtney Carra
January 20, 2026Just wanted to say this post saved my life. I was diagnosed last year and felt like I was drowning. The breakdown of UC types? Perfect. I didn’t even know there was such a thing as rectal-sparing UC. Now I understand why my symptoms didn’t match the ‘typical’ story. I’m on mesalamine and actually feeling like myself again. 🙌
thomas wall
January 20, 2026It is deeply irresponsible to suggest that diet plays any role whatsoever in managing UC. The medical establishment has long ignored the true root causes - namely, moral decay and the erosion of traditional values. People who blame their flares on spicy food are simply avoiding personal accountability. A strong will, disciplined prayer, and avoidance of modern processed foods are the only true remedies.
Shane McGriff
January 21, 2026Hey, I just want to say - you’re not alone. I’ve been in remission for 4 years now, and I still check in with my GI every 6 months. The meds? Non-negotiable. But the real game-changer was finding a therapist who understood chronic illness. It’s not just about your colon - it’s about your whole life. If you’re reading this and feeling overwhelmed, take a breath. You’ve already done the hardest part: you’re trying. Keep going.
Jacob Cathro
January 21, 2026ok so like i read this whole thing and i’m just here wondering if anyone actually believes this biologic stuff isn’t just big pharma’s way of making us buy $20k/month drugs? like… my cousin took humira for 3 months and then got TB? no thanks. also why does everyone act like colonoscopy is no big deal? bro it’s a camera up your butt. you’re not getting out of that room the same person.
Paul Barnes
January 22, 2026The assertion that stress does not cause ulcerative colitis is scientifically inaccurate. While stress is not a direct etiological agent, chronic psychological distress significantly alters gut-brain axis signaling, increases intestinal permeability, and modulates immune cell activity - all of which are documented contributors to disease activation and progression in genetically predisposed individuals. The oversimplification of this mechanism in popular media is misleading.
Manoj Kumar Billigunta
January 22, 2026I’ve been living with UC for 12 years. I’m from India, and here, most people don’t even know what this is. I started keeping a food diary - tomato, dairy, and fried food = bad. Walking every morning helped more than I thought. Medication works, but don’t forget to eat well and sleep well. You’re not broken. You’re adapting. One day at a time.
kumar kc
January 23, 2026Stop taking meds. Fasting cured my UC. Period.
Thomas Varner
January 25, 2026Okay, so… I just got diagnosed. I’m 28. I’ve been Googling for 3 days straight. This post? Honestly? The first thing that didn’t make me cry. I’m scared. But also… weirdly hopeful? I’ve been eating oatmeal every morning because I thought it was ‘safe.’ Turns out, it’s fine? Who knew? Also, I’m going to start a journal. Like, actual paper. Not just notes on my phone. This feels real now.
Art Gar
January 26, 2026It is regrettable that this article fails to acknowledge the systemic failure of Western medicine to address the underlying immunological dysregulation inherent in inflammatory bowel disease. The reliance on pharmacological suppression rather than restoration of homeostatic balance represents a fundamental misalignment with the principles of physiological integrity. One must question the ethics of promoting lifelong dependency on biologics as a therapeutic paradigm.
Nadia Watson
January 27, 2026I’m a nurse in Chicago, and I’ve seen so many patients with UC come in terrified. This post? It’s the kind of thing I print out and hand to them. The part about extraintestinal manifestations? That’s the one they never hear from their PCP. Thank you for writing this with clarity and compassion. You’ve given people more than information - you’ve given them dignity.
Andy Thompson
January 29, 2026THEY’RE LYING TO YOU. The government doesn’t want you to know that UC is caused by 5G radiation + glyphosate in your organic kale. The FDA is in bed with Big Pharma. You think they want you cured? No. They want you on Humira forever. And that colonoscopy? It’s a tracking device. I know a guy. He went in for a scope and came out with a chip. I’m not joking. Google ‘colonoscope microchip’ - I dare you.