5 Oct 2025
- 19 Comments
Biltricide vs Alternative Anthelmintics Comparison Tool
Biltricide (Praziquantel)
Key Indications: Schistosomiasis, taeniasis, diphyllobothriasis
Typical Dose: 40 mg/kg in two doses 4-6 hours apart
Efficacy: 90-95%
Common Side Effects: Nausea, headache, dizziness
Cost: $4-$6 per course
Resistance Risk: Low to moderate
Important Notes:
- Biltricide is the first-line therapy for schistosomiasis and most tapeworm infections.
- Albendazole and mebendazole are effective for soil-transmitted helminths but less effective against schistosomes.
- Ivermectin is ideal for strongyloidiasis and onchocerciasis but not reliable alone for schistosomiasis.
- Nitazoxanide offers broad-spectrum coverage but at a higher cost.
When treating schistosomiasis or tapeworm infections, Biltricide is a branded formulation of praziquantel, an anthelmintic that paralyzes adult worms by opening calcium channels in their membranes. The drug is sold in many countries under different trade names, but the active ingredient remains the same. If you’ve ever wondered whether a cheaper generic or a completely different class of medication might work better, you’re not alone. Below we break down how Biltricide stacks up against the most common alternatives, using the criteria patients and clinicians actually care about.
Key Takeaways
- Biltricide (praziquantel) is the first‑line therapy for schistosomiasis and most tapeworm infections, offering >90% cure rates.
- Albendazole and mebendazole are useful for soil‑transmitted helminths but have lower efficacy against schistosomes.
- Ivermectin shines for strongyloidiasis and onchocerciasis; it’s not a reliable stand‑alone for schistosomiasis.
- Nitazoxanide provides a broad‑spectrum option for protozoa and some helminths, though its cost is higher.
- Cost, resistance patterns, and side‑effect profiles drive the choice more than brand name alone.
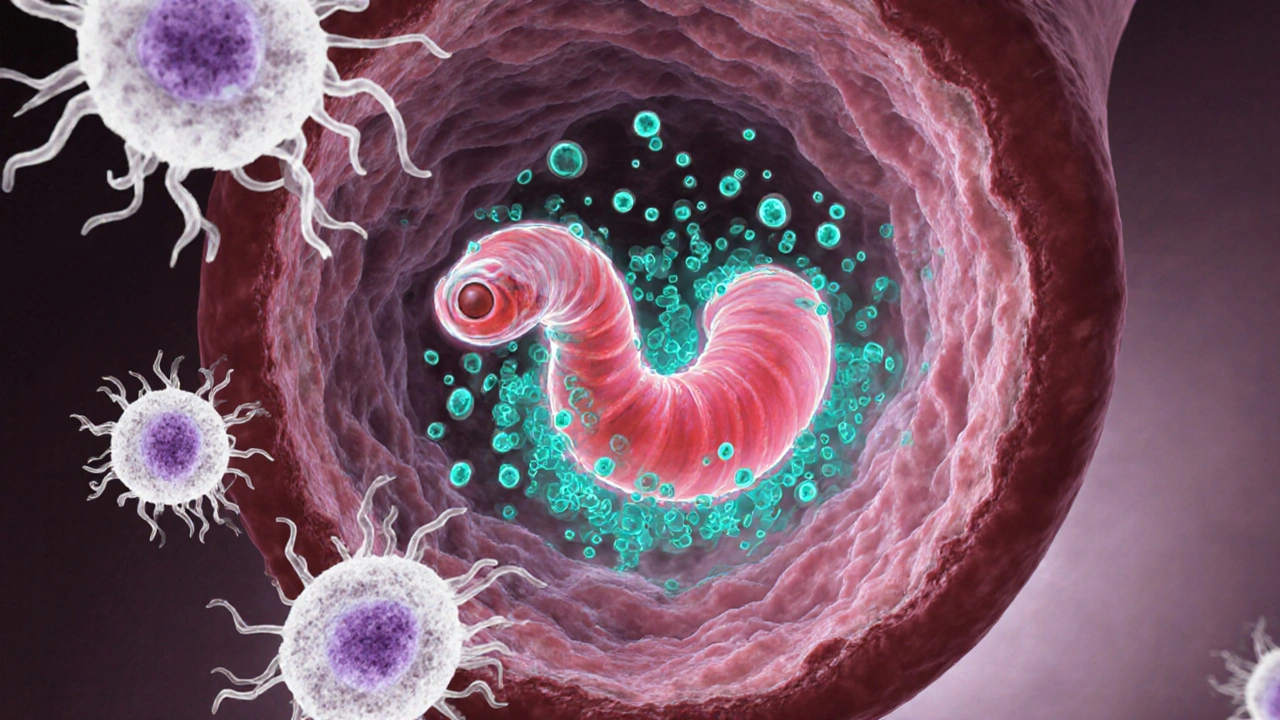
How Biltricide Works
Praziquantel’s mechanism is simple yet powerful: it increases the permeability of the worm’s cell membrane to calcium, causing rapid contraction and paralysis. The immobilized parasite is then dislodged by the host’s immune system and expelled. A typical adult dose is 40mg/kg taken in two divided doses 4-6hours apart. Because the drug targets mature worms, it’s ineffective against early larval stages, which is why timing of treatment matters.
Major Alternatives Overview
Below are the four alternatives that show up most often in prescribing guides and WHO treatment charts.
Albendazole is a benzimidazole that binds to β‑tubulin, inhibiting microtubule formation and starving the parasite. It’s taken as a single 400mg dose for most soil‑transmitted helminths, but higher or repeated dosing is needed for neurocysticercosis.
Mebendazole works the same way as albendazole, disrupting glucose uptake. The standard regimen is 100mg twice daily for three days. It’s praised for its safety in children but has limited activity against schistosomes.
Ivermectin binds to glutamate‑gated chloride channels, leading to paralysis of nematodes. A typical dose is 200µg/kg as a single oral dose. It’s the drug of choice for onchocerciasis and strongyloidiasis, but studies show only modest cure rates for schistosomiasis when used alone.
Nitazoxanide is a synthetic nitrothiazolyl‑salicylamide that interferes with pyruvate‑ferredoxin oxidoreductase. The usual adult dose for intestinal parasites is 500mg twice daily for three days. It’s broad‑spectrum, covering protozoa and some helminths, but price can be a barrier in low‑resource settings.
Comparison Criteria
To make a fair judgement we evaluated each drug on five pillars that matter most in clinical practice.
- Efficacy against target parasites - measured by cure or egg‑reduction rates in controlled trials.
- Safety and tolerability - frequency and severity of side effects, especially in children and pregnant women.
- Dosage convenience - number of tablets, split‑dose requirements, and need for food.
- Cost per treatment course - based on 2024 average wholesale prices in USD.
- Resistance risk - documented cases of reduced susceptibility in endemic regions.
Side‑by‑Side Comparison Table
| Drug | Generic name | Key indications | Typical adult dose | Efficacy* (%) | Common side effects | Cost per course (USD) |
|---|---|---|---|---|---|---|
| Biltricide | Praziquantel | Schistosomiasis, taeniasis, diphyllobothriasis | 40mg/kg in two doses 4-6h apart | 90‑95 | Nausea, headache, dizziness | 4‑6 |
| Albendazole | Albendazole | Hookworm, Ascaris, Trichuris, neurocysticercosis | 400mg single dose (or 400mg daily × 3days) | 70‑85 (schisto<50) | Abdominal pain, rash | 2‑3 |
| Mebendazole | Mebendazole | Roundworm, whipworm, hookworm | 100mg twice daily × 3days | 65‑80 (schisto≈30) | Loose stools, mild liver enzyme rise | 1‑2 |
| Ivermectin | Ivermectin | Onchocerciasis, strongyloidiasis, scabies | 200µg/kg single dose | 50‑70 (schisto≈55) | Pruritus, mild fever | 3‑5 |
| Nitazoxanide | Nitazoxanide | Giardia, Cryptosporidium, some helminths | 500mg twice daily × 3days | 60‑80 (schisto≈65) | Upper‑abdominal discomfort, metallic taste | 8‑12 |
*Efficacy numbers are median cure rates reported in peer‑reviewed trials up to 2024. Exact figures vary by species, infection intensity, and regional resistance patterns.
When to Choose Biltricide Over Others
If you’re dealing with confirmed schistosomiasis (S.mansoni, S.haematobium, or S.japonicum), Biltricide remains the gold standard. Its high cure rate, short treatment window, and single‑to‑double‑dose regimen make it hard to beat. In pregnant women beyond the first trimester, the drug is still considered safe; for earlier pregnancy, many clinicians switch to albendazole only if the risk outweighs the benefit.
For mixed infections-say, a traveler with both hookworm and a light tapeworm-combining albendazole (for hookworm) with a single dose of Biltricide can clear both parasites efficiently. However, in cases where ivermectin is already indicated (e.g., strongyloidiasis co‑infection), adding praziquantel may be unnecessary unless schistosomiasis testing is positive.
Cost‑sensitive settings often rely on generic praziquantel powder, which can be as cheap as $1‑2 per course. That price advantage keeps Biltricide competitive even when alternative drugs are available as generics.
Practical Tips & Common Pitfalls
- Take with food - a fatty meal improves praziquantel absorption by up to 40%.
- Check for liver disease - while the drug is generally safe, severe hepatic impairment can increase side‑effect severity.
- Watch for resistance - in parts of East Africa, reduced praziquantel efficacy has been reported; routine follow‑up stool exams are advised.
- Avoid monotherapy for mixed helminths - pairing praziquantel with albendazole or ivermectin covers a broader spectrum.
- Pregnancy timing - if treatment must occur in the first trimester, discuss risks and consider albendazole only if diagnosis is certain.
Next Steps for Patients and Clinicians
1. Confirm diagnosis with stool microscopy or antigen testing.
2. Choose the drug based on the infection type, local resistance data, and patient-specific factors (age, pregnancy, liver function).
3. Counsel the patient to take the dose with a fatty snack and to expect mild, transient side effects.
4. Schedule a follow‑up exam 4-6weeks later to verify egg clearance.
5. In endemic areas, consider mass drug administration of praziquantel as part of community‑wide control programs.
Frequently Asked Questions
Is Biltricide safe for children?
Yes. The WHO recommends a 40mg/kg dose for children aged 2years and older. Side effects are usually mild (headache, abdominal discomfort) and resolve within a day.
Can I use albendazole instead of Praziquantel for tapeworms?
Albendazole works for some tapeworm species but is less effective against Taenia solium and Diphyllobothrium. Praziquantel cures >90% of these infections, so it remains the preferred choice.
What should I do if I miss a Biltricide dose?
Take the missed dose as soon as you remember, then continue with the remaining schedule. If it’s already time for the second dose, don’t double‑up; just proceed with the next dose at the planned interval.
Are there any drug‑interaction concerns?
Praziquantel is metabolized by CYP3A4. Concomitant use of strong CYP3A4 inhibitors (e.g., ketoconazole) can increase blood levels and intensify side effects. Adjust dosing or monitor closely if such agents are required.
How does resistance to praziquantel develop?
Resistance is linked to mutations in the parasite’s calcium‑channel genes that reduce drug binding. Repeated sub‑therapeutic dosing in mass‑treatment programs can select for these strains. Rotating with alternative anthelmintics or combining drugs helps slow resistance.
By weighing efficacy, safety, cost, and local resistance patterns, you can decide whether Biltricide stays on the shelf or an alternative takes its place. The right choice not only clears the current infection but also protects your community from future outbreaks.


april wang
October 5, 2025Thank you for sharing this comprehensive comparison; it offers a solid foundation for clinicians and patients alike. The detailed breakdown of efficacy, dosage, and side‑effect profiles really helps demystify why Biltricide remains the first‑line choice for schistosomiasis. I especially appreciate the inclusion of resistance risk, since emerging data from endemic regions suggest that sub‑therapeutic dosing can foster resistant strains. Moreover, the cost analysis is valuable for health‑systems operating under tight budgets, highlighting that a $4‑$6 course is often more feasible than the pricier nitazoxanide. The table format makes it easy to scan, but I would suggest adding a column for pregnancy safety, as that’s a frequent concern among practitioners. While albendazole and mebendazole are excellent for soil‑transmitted helminths, their limited activity against adult schistosomes underscores the importance of matching drug to parasite life cycle. I also note that ivermectin’s modest efficacy against schistosomiasis might improve when combined with praziquantel, a strategy worth exploring in mass‑treatment campaigns. The discussion about CYP3A4 interactions is spot‑on; clinicians should be vigilant when patients are on strong inhibitors like ketoconazole. In terms of patient experience, the common side effects of nausea and dizziness are generally mild and transient, but counseling can mitigate adherence issues. It would be beneficial to see a point‑of‑care decision algorithm that incorporates local resistance patterns. Lastly, the brief mention of missed doses could be expanded into a quick FAQ, as many patients forget the second dose. Overall, the post balances scientific rigor with practical guidance, making it a valuable reference for both seasoned infectious disease specialists and frontline health workers.
Vishnu Raghunath
October 6, 2025Oh sure, big pharma just wants us to swallow money‑filled pills while they hide the magic cure in some secret vault.
Lin Zhao
October 7, 2025Great job laying out everything! 😊 The side‑effect list is clear, and the cost comparison really hits home for patients on a budget. 📊 I think adding a quick note about the best time to take Biltricide with food could help avoid those pesky nausea episodes. 🌟 Also, a reminder that kids need weight‑based dosing would be useful for families. 👍
Laneeka Mcrae
October 7, 2025Look, if you’re deciding between these drugs, the numbers speak for themselves: Biltricide's 90‑95% cure rate outperforms albendazole and mebendazole for schistosomiasis. The dosage schedule is simple-just two doses-and the side‑effects are manageable. Don't be swayed by the hype around ivermectin; it’s not reliable for schisto on its own. Cost‑effectiveness also favors Biltricide, making it the sensible choice for public health programs.
Kendra Barnett
October 8, 2025Really solid overview here. The way you highlighted the cost differences makes it easier for clinics to budget. For anyone worried about side effects, remember that they’re usually mild and go away quickly. It’s good to see the emphasis on resistance monitoring-keeping an eye on that helps preserve drug efficacy.
Warren Nelson
October 9, 2025Interesting read. The comparison chart does a good job of summarizing key points without overwhelming detail. I noticed the mention of CYP3A4 interactions; that's a useful heads‑up for patients on other meds. Overall, a balanced look at the options.
Abby Elizabeth
October 10, 2025this is sooo boring lol
Mark Haycox
October 10, 2025Our healthcare system should stick with the proven American drug Biltricide, not waste money on foreign alternatives. The cheap imports like nitazoxanide are just a ploy to undermine our pharma industry.
Michael Taylor
October 11, 2025Wow!!! This post really covers a lot of ground, and I must say, it’s impressive how the author managed to cram so many details into one article!!! The tables are neat, the bullet points are clear, and the explanations are thorough!!! However, I can’t help but notice that the section on ivermectin could have used a bit more depth, especially regarding its limited efficacy against schistosomiasis!!! Also, a quick disclaimer about the need for medical supervision when using these meds would be helpful!!! Overall, fantastic work, keep it up!!!
Troy Brandt
October 12, 2025I really appreciate the effort put into this side‑by‑side analysis; it’s exactly the sort of resource that frontline clinicians need when faced with limited time and resources. By breaking down each drug’s efficacy, safety, dosage convenience, cost, and resistance risk, the author gives a holistic view that can guide treatment decisions in both endemic and non‑endemic settings. The inclusion of practical tips-like taking Biltricide with food to reduce nausea-is a nice touch that bridges the gap between theory and practice. I also like the call for monitoring resistance patterns, as this is crucial for sustaining the effectiveness of praziquantel in mass‑drug‑administration campaigns. One suggestion would be to add a quick reference chart for pediatric dosing, since children are often the most affected by helminth infections. Additionally, a short FAQ on managing missed doses could further enhance usability. Overall, the article balances scientific rigor with user‑friendly presentation, making it a valuable tool for healthcare providers worldwide.
Callum Smyth
October 13, 2025Great point about the cure rates-Biltricide truly stands out. I'd add that in many community treatment programs, its two‑dose regimen improves compliance compared to drugs that require longer courses. This compliance factor often translates into better overall program success.
Thomas Burke
October 13, 2025Thanks for the thorough breakdown; the added note on pregnancy safety would indeed make the guide more complete.
Debbie Frapp
October 14, 2025Nice observation on the CYP3A4 interaction; it's something I’ve seen cause unexpected side effects in patients on antifungal therapy.
Michelle Abbott
October 15, 2025The pharmacokinetic profile of praziquantel, characterized by rapid hepatic metabolism via CYP3A4 isoenzymes, mandates vigilant therapeutic drug monitoring in polypharmacy contexts to mitigate adverse event incidence.
Nilesh Barandwal
October 16, 2025In the grand tapestry of medicine, truth often lies between the shadows of suspicion and the light of evidence.
Elise Smit
October 16, 2025Your use of emojis adds a friendly tone, but the clinical information remains spot‑on and well‑structured.
Sen Đá
October 17, 2025While the analysis is commendable, it neglects the strategic advantage of proprietary formulations that dominate the market, thereby undermining domestic pharmaceutical sovereignty.
Tatiana Akimova
October 18, 2025Exactly-improving adherence is the linchpin of any successful eradication campaign; without it, even the most effective drug fails its purpose.
Calandra Harris
October 19, 2025Indeed the pregnancy safety data could be the deciding factor for many clinicians