Vitamin K: What It Does, Who Needs It, and How Medications Affect It
When you cut yourself, vitamin K, a fat-soluble nutrient critical for blood clotting. Also known as phylloquinone, it’s the reason your cuts stop bleeding instead of turning into a mess. Without enough vitamin K, even a small scrape can take longer to heal—and in rare cases, lead to dangerous internal bleeding. But it’s not just about stopping blood loss. This same nutrient also helps your bones stay strong by activating proteins that bind calcium. If you’re on blood thinners like warfarin, vitamin K becomes even more important—not because you need more of it, but because too much or too little can throw your whole treatment off balance.
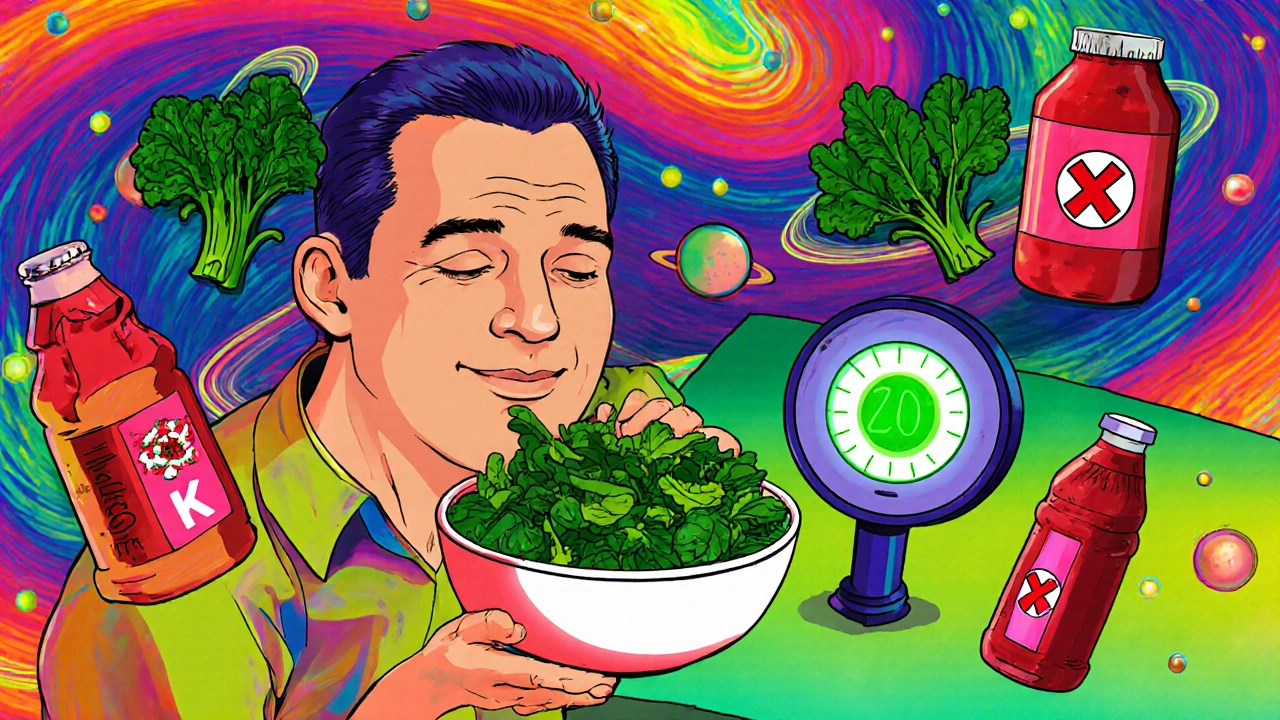
Many people don’t realize how closely vitamin K ties into their medications. For example, if you’re taking warfarin, a blood thinner used to prevent clots in people with atrial fibrillation or artificial heart valves, your doctor monitors your INR levels to make sure your blood isn’t clotting too fast or too slow. Vitamin K directly counters warfarin’s effect. A sudden change in your intake—like eating a big salad one day and none the next—can make your INR swing wildly. That’s why consistency matters more than quantity. You don’t need to avoid leafy greens; you just need to keep them steady. The same goes for anticoagulants, a class of drugs that includes newer options like rivaroxaban and apixaban, which interact less with vitamin K than warfarin. Even if you’re on a newer drug, your body still needs vitamin K for normal function, and deficiencies can show up as bruising, nosebleeds, or even gastrointestinal bleeding.
It’s not just about pills and greens. Antibiotics can wipe out the good bacteria in your gut that make vitamin K, especially with long-term use. That’s why some people on extended antibiotic courses develop low levels, even if they eat plenty of kale or broccoli. Older adults, people with digestive diseases like Crohn’s or celiac, and those who’ve had gastric bypass surgery are also at higher risk. And while supplements exist, most healthy people get enough from food—kale, spinach, Brussels sprouts, soybean oil, and even some cheeses. The key isn’t to load up on supplements unless your doctor says so. Too much vitamin K from supplements can interfere with treatment, and there’s no proven benefit for people who aren’t deficient.
What you’ll find below are real, practical posts that dig into how vitamin K plays out in daily life—with medications, in aging bodies, and in situations most guides ignore. You’ll see how it connects to warfarin dosing, why some people react differently to generics, how antibiotics can quietly mess with your nutrient levels, and what to do if you’re on blood thinners and suddenly can’t eat your usual greens. This isn’t theory. It’s what people actually deal with when managing their health.
Warfarin Food Interactions: Complete Food List and Guidelines for Safe Use
Learn which foods affect warfarin, how to eat safely without giving up vegetables, and what to avoid to prevent dangerous bleeding or clotting. Keep your INR stable with consistent diet habits.