Prolactin: What It Is and Why It Matters
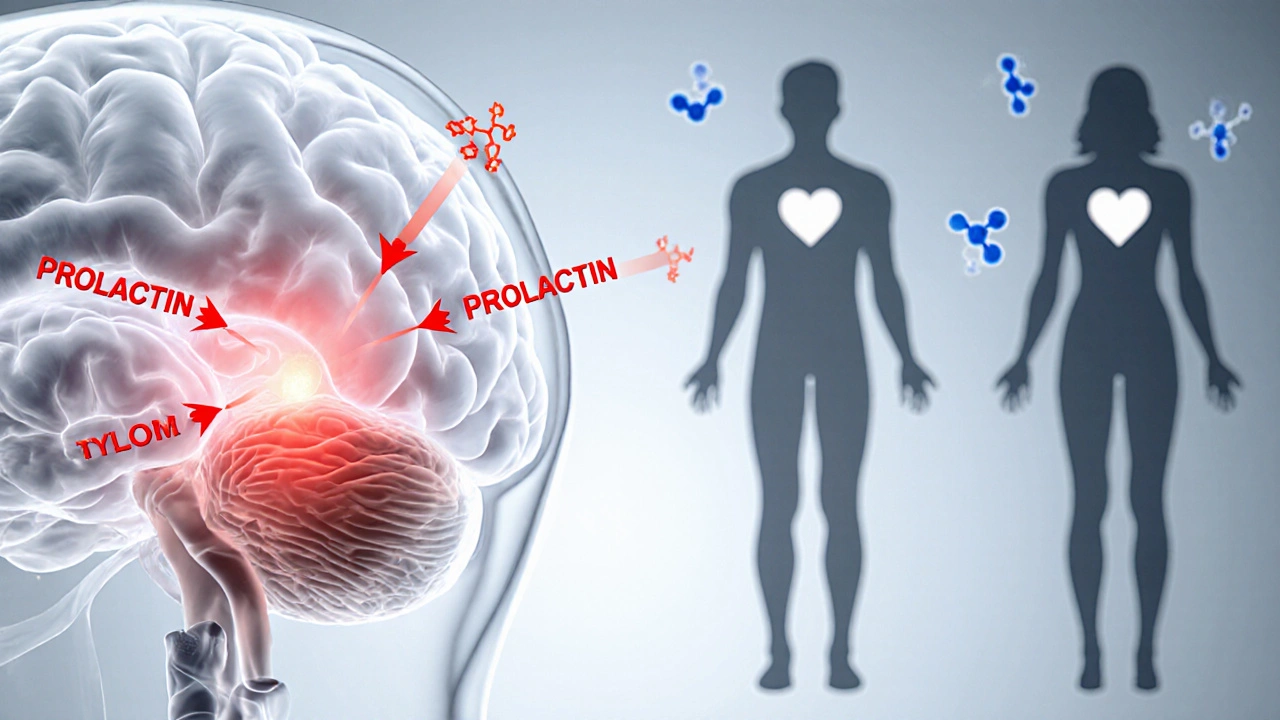
When you hear prolactin, a protein hormone released by the anterior pituitary that primarily triggers milk production after birth. Also known as lactogenic hormone, it influences metabolism, immune function, and the reproductive system. Prolactin isn’t just for nursing moms; men and non‑pregnant women have it too, and the amount circulating in the bloodstream tells your body a lot about endocrine health. The hormone’s production is tightly controlled by dopamine, a brain chemical that tells the pituitary to keep prolactin levels low unless breastfeeding signals a rise. When that balance tips, you can see a range of symptoms—from breast tenderness and unwanted milk flow to irregular periods and reduced libido. Understanding this hormone’s role lays the groundwork for spotting problems early and choosing the right care path.
Key Topics Covered
One of the most common disruptions is hyperprolactinemia, a condition where prolactin levels stay higher than normal without a nursing trigger. It can stem from a tiny pituitary tumor called a prolactinoma, certain medications, stress, or hypothyroidism. The pituitary gland, the master endocrine organ perched at the base of the brain is central here: any growth or inflammation can push the gland to overproduce prolactin. Symptoms often overlap with other reproductive issues, making diagnosis a bit of detective work. Blood tests are the first step—doctors draw a sample in the morning, when levels are most stable, and compare it to reference ranges. If numbers are high, imaging like MRI may be ordered to check for a prolactinoma. Meanwhile, clinicians look at the bigger picture: high prolactin can suppress the release of gonadotropin‑releasing hormone, leading to low estrogen or testosterone, which then causes infertility, menstrual disturbances, or erectile dysfunction. Recognizing these links helps patients and providers decide whether medication, surgery, or lifestyle tweaks are needed.
Treatment usually starts with dopamine agonist, a drug class that mimics dopamine’s inhibitory effect on prolactin secretion such as cabergoline or bromocriptine. These medicines can lower prolactin by up to 90 % and often shrink small tumors, easing pressure on surrounding brain tissue. Side effects are generally mild—nausea, dizziness, or low blood pressure—but patients should report any mood changes promptly. For those who can’t tolerate medication, surgery to remove a prolactinoma is an option, though it’s less common because drugs work well in most cases. Lifestyle adjustments also play a role: reducing stress, avoiding estrogen‑boosting supplements, and managing thyroid health can keep prolactin in check. Monitoring is an ongoing process; regular blood work ensures levels stay within target ranges and helps catch a rebound early. By linking hormone testing, the anatomy of the pituitary, and targeted therapies, you get a clear roadmap to restore balance and protect fertility. Below you’ll find articles that dive deeper into each of these areas, offering practical tips, detailed drug comparisons, and the latest guidance on managing prolactin‑related health concerns.
How Hyperprolactinaemia Impacts Libido and Sexual Function
Explore how high prolactin levels affect libido and sexual function, learn to diagnose the issue, and discover effective treatments and lifestyle tips for recovery.