Food Interactions: How What You Eat Affects Your Medications
When you take a pill, it doesn’t just disappear into your system like magic—it has to fight its way through your stomach, your gut, and your liver, and food interactions, how what you eat changes how your body handles drugs. Also known as diet-drug interactions, these can make your medicine less effective, more toxic, or even cause serious side effects. It’s not just about skipping meals. A glass of grapefruit juice, a bowl of spinach, or even a cup of coffee can change how your body absorbs or breaks down your drugs.
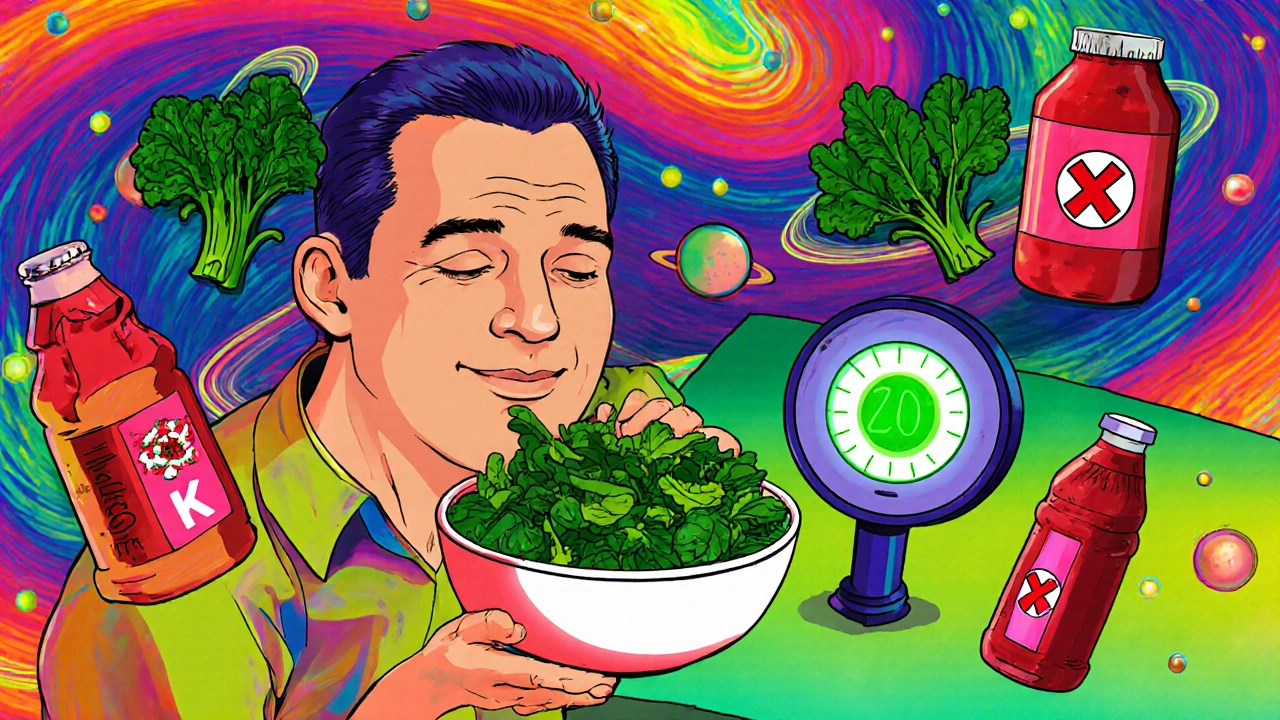
Take levothyroxine, a thyroid hormone replacement used to treat hypothyroidism. If you take it with breakfast—especially with calcium, soy, or fiber-rich foods—it barely gets absorbed. That means your thyroid levels stay low, and you keep feeling tired, cold, and sluggish. The fix? Take it on an empty stomach, wait 30 to 60 minutes before eating. Same with warfarin, a blood thinner that’s super sensitive to vitamin K. One day you eat a big salad, the next you eat pasta—your blood clotting time swings wildly. Doctors don’t tell you this often, but consistency matters more than perfection.
Then there’s alcohol and medications, a dangerous mix that can overload your liver, spike drowsiness, or cause internal bleeding. Mixing alcohol with painkillers like acetaminophen? Liver damage. With antidepressants? Worse mood swings. With blood pressure meds? Dizziness that lands you in the ER. And it’s not just booze—some herbal teas, energy drinks, and even black licorice can interfere with your meds. You don’t need to give up everything, but you do need to know which combos to avoid.
It’s not just about avoiding bad pairings. Timing matters too. Some drugs need space before or after meals. Others need to be taken with food to reduce stomach upset. And if you’re on multiple meds, the chances of one food item messing with two or more drugs go up fast. That’s why keeping a simple log—what you ate, when you took your pills, and how you felt—can be more helpful than you think.
What you’ll find below isn’t theory. It’s real stories from people who learned the hard way. Someone who stopped feeling better after switching to generic levothyroxine—until they realized their morning smoothie was blocking absorption. Someone who thought a glass of wine at dinner was fine—until they ended up in the hospital with a dangerous heart rhythm after taking azithromycin. These aren’t rare cases. They’re common mistakes, hidden in plain sight.
Vitamin C and Iron: How to Maximize Absorption and Avoid Drug Interactions
Vitamin C boosts iron absorption by turning hard-to-absorb iron into a form your body can use. Pairing 100-200mg of vitamin C with plant-based iron meals can double uptake-but timing and avoiding blockers like calcium and coffee are critical.
Warfarin Food Interactions: Complete Food List and Guidelines for Safe Use
Learn which foods affect warfarin, how to eat safely without giving up vegetables, and what to avoid to prevent dangerous bleeding or clotting. Keep your INR stable with consistent diet habits.