Takayasu's Arteritis: What You Need to Know
If a doctor ever mentions "large‑vessel vasculitis," they might be talking about Takayasu's arteritis. It’s a rare condition that inflames the big arteries, especially the aorta and its main branches. Most patients are women under 40, but anyone can get it. Knowing the basics helps you catch problems early and work with your doctor on a solid plan.
What is Takayasu's Arteritis?
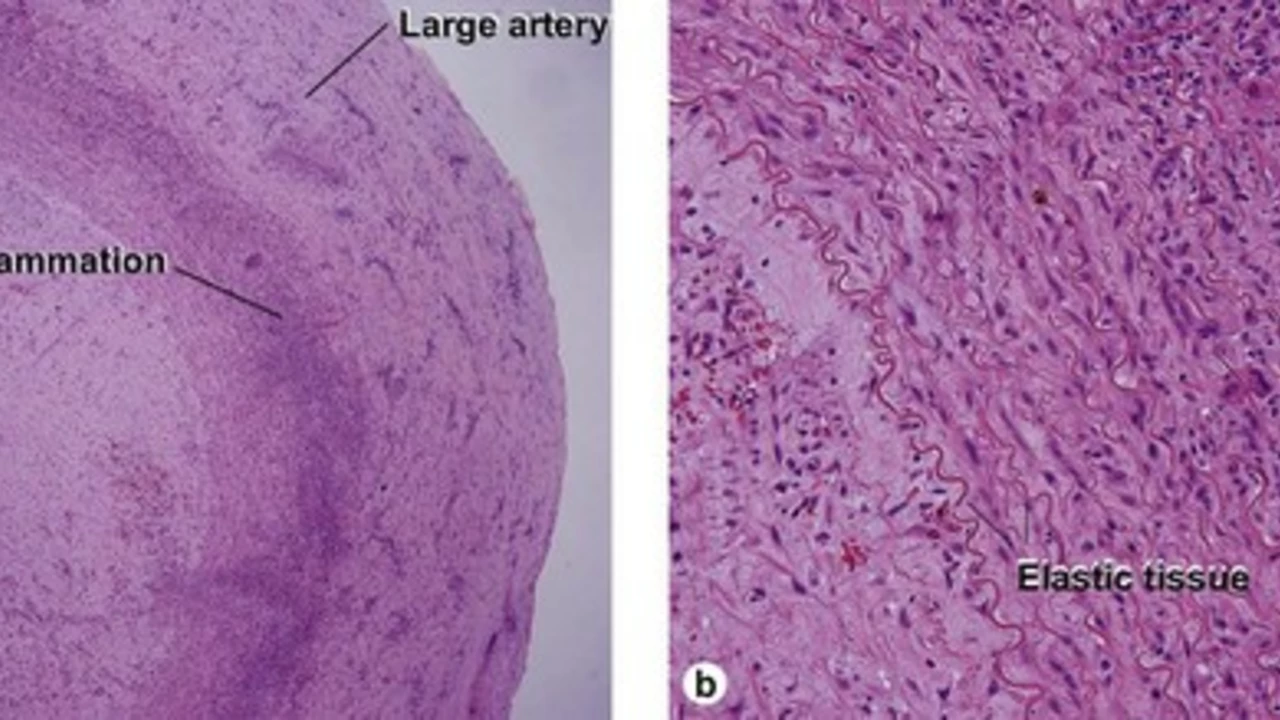
Think of your arteries as flexible tubes that carry blood everywhere. In Takayasu's arteritis those tubes become thick, scarred, and narrowed because the immune system attacks them by mistake. The inflammation can cause pain, reduced blood flow, or even blockages that affect organs like the heart, brain, or kidneys.
Because it’s rare, symptoms often get missed or blamed on something else. Common clues include:
- Persistent fever or night sweats
- Unexplained weight loss
- Weak pulse in one arm or leg
- Chest or back pain that doesn’t go away
- Headaches, dizziness, or vision changes
If you notice any of these for more than a few weeks, especially with a weak pulse on one side, it’s worth asking your doctor about possible artery inflammation.
How Doctors Diagnose It
The first step is a thorough physical exam. Your clinician will feel for differences in blood pressure between arms and listen for murmurs that suggest narrowed vessels. Blood tests can show markers of inflammation, like an elevated ESR or CRP, but they don’t confirm the disease on their own.
Imaging does the heavy lifting. Ultrasound can spot thickened artery walls, while CT angiography or MR angiography gives a detailed view of blockages and aneurysms. In some cases, doctors use PET scans to highlight active inflammation.
The diagnosis is usually made by combining your symptoms, lab results, and imaging findings. Because the disease can mimic other conditions, a specialist—often a rheumatologist or vascular surgeon—is involved.
Managing Takayasu's Arteritis
Treatment aims to calm the immune attack and keep arteries open. The first line is high‑dose corticosteroids (like prednisone) to reduce inflammation quickly. Most patients need steroids for several months, then a slow taper.
Because long‑term steroid use brings side effects, doctors add “steroid‑sparing” drugs called DMARDs (disease‑modifying antirheumatic drugs). Common choices are methotrexate, azathioprine, or mycophenolate. In recent years, biologic agents such as tocilizumab—an IL‑6 inhibitor—have shown good results for people who don’t respond to traditional meds.
Regular monitoring is key. You’ll likely have blood tests every few months and repeat imaging every 6–12 months to see how the arteries are healing or if new blockages appear.
Lifestyle tweaks also help. A balanced diet, low in sodium and saturated fats, protects heart health. Gentle exercise improves circulation without stressing inflamed vessels. If you smoke, quitting is a must—smoking worsens vascular damage.
Living with the Condition
Many people lead active lives after diagnosis. The trick is staying on top of follow‑up appointments and medication schedules. Keep a symptom diary; noting changes in pulse strength or new pain can alert your doctor to flare‑ups before they become serious.
If you’re pregnant or planning a pregnancy, discuss it early with your care team. Some medications need adjustment, but many women successfully manage the disease through pregnancy.
Support groups—online or in‑person—offer practical tips and emotional comfort. Hearing stories from others who’ve navigated surgery, medication changes, or daily challenges can be reassuring.
Takayasu's arteritis may feel overwhelming at first, but with early detection, the right meds, and regular monitoring you can keep it under control and focus on what matters most in life.
The Benefits of Atorvastatin for Patients with Takayasu's Arteritis
In recent studies, I've discovered the numerous benefits of Atorvastatin for patients with Takayasu's Arteritis. This medication, commonly used to lower cholesterol, has shown promising results in reducing inflammation and improving arterial wall thickness in these patients. Furthermore, Atorvastatin has been found to lower the risk of cardiovascular events and improve overall quality of life for those suffering from this rare autoimmune disease. With minimal side effects, this drug offers a safer alternative to other immunosuppressive therapies. I encourage those affected by Takayasu's Arteritis to consult with their healthcare providers about the potential benefits of Atorvastatin.