Orthostatic Hypotension: Causes, Risks, and Medication Links
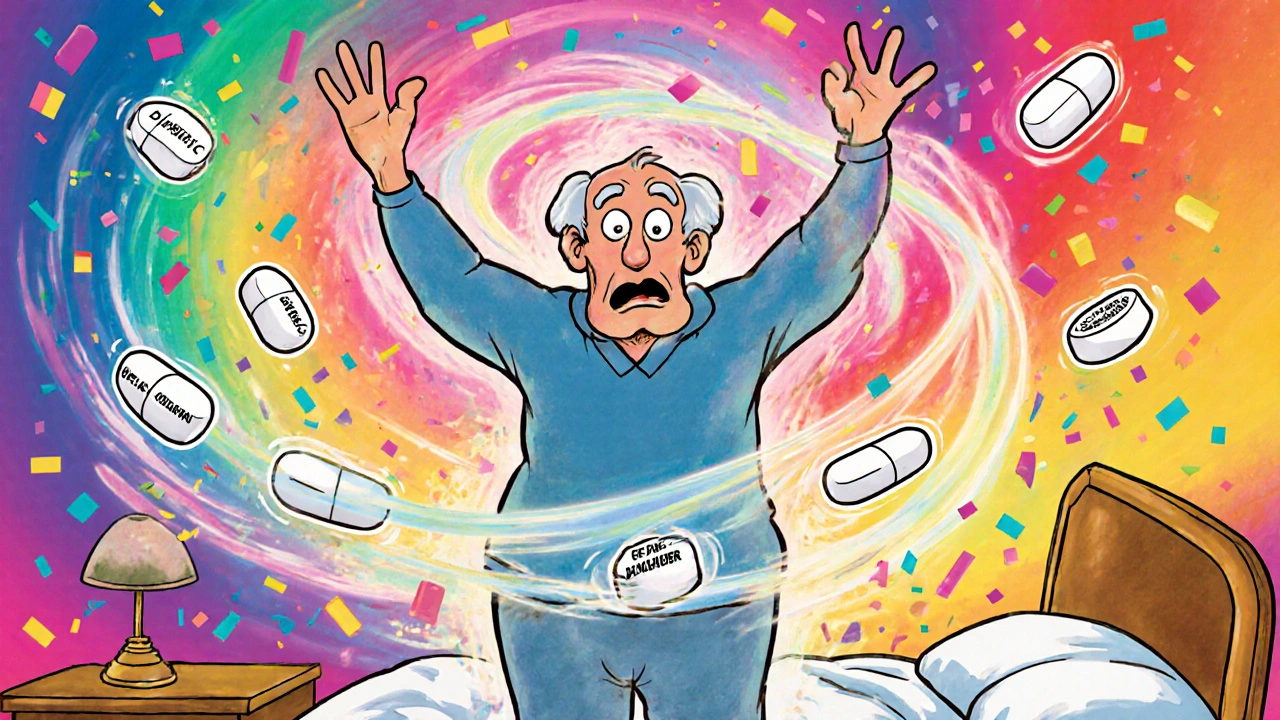
When you stand up and feel dizzy, lightheaded, or like you might pass out, you’re likely experiencing orthostatic hypotension, a sudden drop in blood pressure upon standing that reduces blood flow to the brain. Also known as postural hypotension, it’s not just an old-age quirk—it’s often tied to medications, dehydration, or underlying conditions that affect how your body regulates blood flow. This isn’t just about feeling a little woozy. If your blood pressure drops too fast when you stand, you’re at higher risk for falls, injuries, and even fainting—especially if you’re on blood pressure meds, diuretics, or antidepressants.
Many of the drugs people take daily can make this worse. For example, SSRIs, common antidepressants used for depression and anxiety, can interfere with blood pressure control and are linked to hyponatremia, a dangerous drop in blood sodium that further lowers blood pressure. Warfarin, a blood thinner that requires careful diet and monitoring, doesn’t directly cause orthostatic hypotension, but if it leads to internal bleeding or low blood volume, the risk spikes. And if you’re taking levothyroxine, a thyroid hormone replacement that affects metabolism and heart function, even small dosing errors can throw off your circulation and make standing up feel like a workout.
One of the most direct links comes from idiopathic orthostatic hypotension, a condition where the body’s ability to regulate blood pressure fails without a clear cause. Research shows low blood volume is often the root issue—meaning you’re not just dizzy because you’re old, but because your body simply doesn’t have enough fluid circulating to keep up with position changes. That’s why drinking more water, wearing compression socks, or adjusting salt intake can help more than you’d think. But if you’re on multiple meds, especially those that affect your heart, kidneys, or nerves, the problem gets layered. Macrolide antibiotics, for instance, don’t cause this directly, but if they trigger heart rhythm issues, your body’s ability to compensate for standing drops even further.
What you’ll find below isn’t just a list of articles—it’s a practical toolkit. From how to track which meds are making your dizziness worse, to how to safely adjust your routine without risking a fall, these posts give you real, tested strategies. You’ll see how blood volume ties into treatment, why some people react differently to generics, and how simple changes in timing or diet can make a measurable difference. No fluff. No guesswork. Just what works when your blood pressure drops the moment you stand up.
Orthostatic Hypotension from Medications: Why You Feel Dizzy When You Stand Up
Dizziness when standing up? It could be your medications. Learn which drugs cause orthostatic hypotension, how to spot it, and what steps you can take to feel safer on your feet.