9 Feb 2026
- 14 Comments
Autoimmune hepatitis isn't just another liver problem. It’s when your immune system, the very thing meant to protect you, turns on your liver and starts attacking it. No virus. No alcohol. No fatty diet. Just your own body doing the damage. Left untreated, it can lead to scarring, liver failure, or even the need for a transplant. But here’s the good news: with the right diagnosis and treatment, most people can stop the damage and even reverse it. The keys? Corticosteroids like prednisone and azathioprine. Together, they’ve been saving lives since the 1970s.
How Do You Know You Have It?
| Category | Key Indicator | Threshold |
|---|---|---|
| Serology | Antinuclear antibodies (ANA) or SMA | ≥1:40 titer |
| Serology | IgG level | ≥1.5x upper limit of normal |
| Histology | Interface hepatitis | Present in ≥20 portal tracts |
| Exclusion | Viral hepatitis | Must be ruled out |
| Scoring | Revised IAIHG score | ≥15 = probable, ≥20 = definite |
No single test confirms autoimmune hepatitis. It’s a puzzle. Doctors look at blood markers, liver biopsy results, and rule out other causes like hepatitis B or C. Elevated ALT and AST - often 5 to 10 times higher than normal - are red flags. So is a spike in IgG, the antibody your body overproduces in this disease. But the real clincher? A liver biopsy. It shows the telltale sign: interface hepatitis, where immune cells swarm the border between liver tissue and blood vessels. Without this, diagnosis isn’t complete.
The 2025 European guidelines dropped the old habit of splitting AIH into Type 1 and Type 2 based on antibody patterns. Why? Because whether you test positive for ANA, SMA, or LKM1 doesn’t change how you’re treated. The treatment is the same. This simplifies things for doctors and patients alike.
Why Steroids Are the First Line
Prednisone (or its cousin prednisolone) is the first drug you’ll likely be put on. It works fast. In fact, 80-90% of patients show improvement in liver enzymes within two weeks. That’s unusually quick for an autoimmune disease. It’s one reason doctors suspect AIH when they see it.
The starting dose? Usually 0.5 to 1 mg per kilogram of body weight - up to 60 mg daily. That’s a lot. And it comes with side effects: weight gain, mood swings, trouble sleeping, and a rounder face - what some call “moon face.” But here’s the trick: you don’t stay on this dose forever. The goal is to taper it down to 10-15 mg per day by week 8. That’s the plan. And it works.
Why taper? Because long-term steroid use is risky. After five years, 15% of patients develop diabetes, 20% lose bone density, and 10% get cataracts. That’s why doctors pair it with azathioprine - not just to help, but to let you get off the steroids faster.
Azathioprine: The Steroid-Sparing Partner
Azathioprine (brand name Imuran) doesn’t work fast. It takes months. But it’s the reason many people can eventually live on just 5 mg of prednisone - or even none at all. It suppresses the immune system differently than steroids, targeting the cells that cause the attack. When used together, steroid side effects drop from 70% to 30%.
The dose starts low - 50 mg daily - and slowly increases to 1-2 mg per kg (up to 150 mg). But before you even start, there’s a critical step: testing for TPMT enzyme levels. About 0.3% of people have a genetic variant that makes azathioprine dangerously toxic. Without this test, they risk life-threatening bone marrow suppression. In Europe, 78% of centers do this test. In the U.S., it’s only 45%. That gap needs to close.
Side effects of azathioprine? Nausea, fatigue, and sometimes pancreatitis. One patient on Reddit described going from 100 mg to complete withdrawal because of severe pancreatitis. That’s rare, but it happens. That’s why blood counts are checked every few weeks early on.

What Does Success Look Like?
Success isn’t just feeling better. It’s what the numbers say. Complete biochemical response means ALT and AST return to normal, and IgG levels drop. This happens in 60-80% of patients within 18 to 24 months. But the real win? Histological remission. That means the liver biopsy, repeated after 2-3 years, shows no more interface hepatitis. That’s what doctors aim for - and it happens in 50-70% of those who stick with treatment.
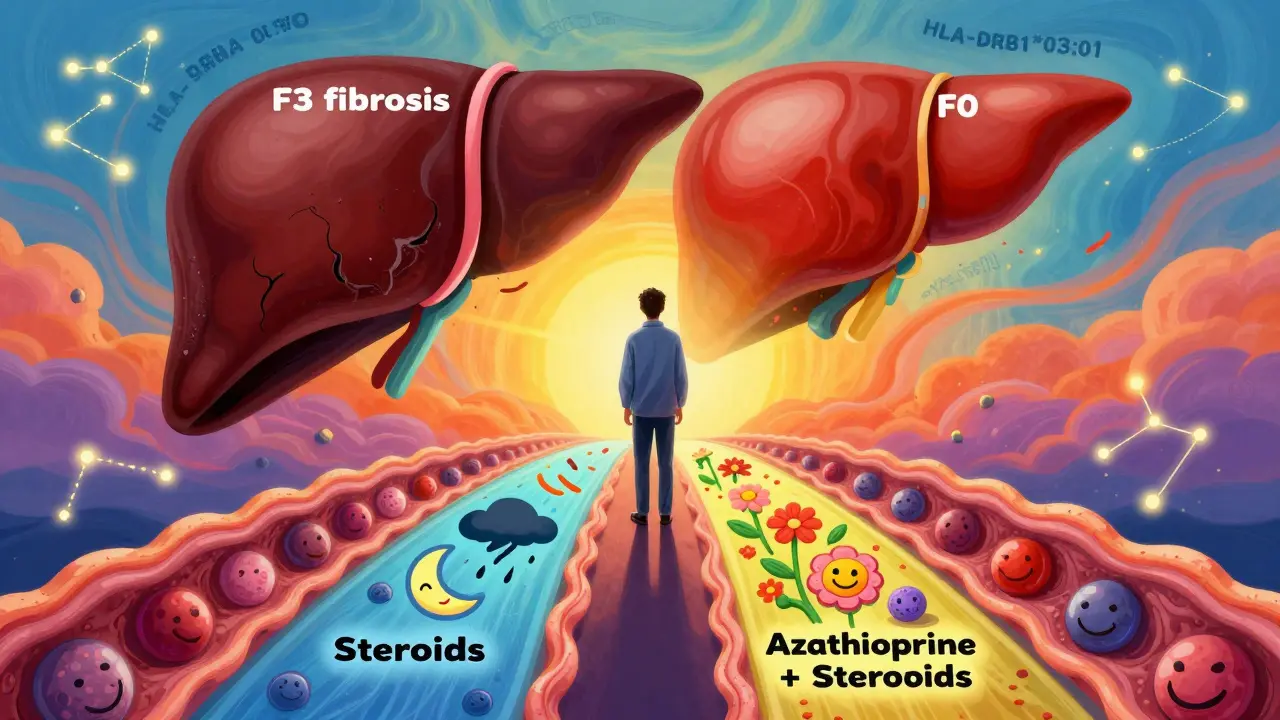
One patient on HealthUnlocked shared: “After two years on 5mg prednisone and 75mg azathioprine, my biopsy went from F3 fibrosis to F0 - no scarring left.” That’s not a miracle. It’s science. The liver can heal - if you catch it early and treat it right.
What If Treatment Doesn’t Work?
One in ten patients don’t respond. Or they can’t tolerate the side effects. That’s when second-line drugs come in.
- Mycophenolate mofetil (CellCept): Used in 25-30% of refractory cases. Better GI tolerance than azathioprine for some. Dose: 1-1.5 grams twice daily.
- Calcineurin inhibitors (tacrolimus, cyclosporine): For those who can’t use azathioprine or mycophenolate. Need careful blood level monitoring.
- New options on the horizon: JAK inhibitors like tofacitinib and IL-6 blockers like clazakizumab are showing promise in trials. One phase 2 trial reported 55% response rates. These aren’t standard yet - but they’re coming.
And there’s new hope. The FDA granted breakthrough therapy status to obeticholic acid (Ocaliva) for AIH. Phase 3 trials showed a 42% complete response rate - better than standard therapy. It’s not approved yet, but it’s close.
Long-Term Management and Relapse Risk
This isn’t a short-term fix. Most people need maintenance therapy for years - sometimes for life. Why? Because stopping treatment too soon is risky. Between 50% and 90% of patients relapse after stopping meds. That’s why doctors don’t rush to stop.
Some try to taper off after 2-3 years of full remission. But even then, 70% of relapses happen within three months of stopping. That’s why tapering is slow - over 6 to 12 months - and why liver enzymes are watched like a hawk after stopping.
And don’t forget vaccinations. If you’re on immunosuppressants, your body won’t respond well to vaccines. Get hepatitis A and B shots before starting treatment. Once you’re on steroids or azathioprine, vaccine effectiveness drops from 90% to 40-60%.
Monitoring and Prevention
Regular blood tests are non-negotiable. Every 2-4 weeks during the first few months. Then every 3 months. IgG every quarter. Liver enzymes every time. And before you start, you must be tested for hepatitis B. Why? Because immunosuppressants can wake up a hidden HBV infection - and that can be deadly. If you’re positive, you’ll need antivirals like tenofovir on top of your AIH treatment.
TPMT testing is now standard in academic centers. It’s not expensive - $250 to $400 in the U.S. - but it prevents disaster. If your enzyme level is low or absent, azathioprine is off the table. Alternatives exist. But skipping this test? That’s a gamble with your life.
What Patients Are Really Saying
On forums like Reddit and the American Liver Foundation, patients don’t talk about numbers. They talk about life.
“Moon face. 30 pounds of fluid in three weeks. Insomnia that felt permanent.” That’s steroid side effects. “Azathioprine gave me pancreatitis. Switched to mycophenolate. Finally, my liver enzymes stabilized after 18 months.” That’s the trial-and-error reality.
But then there’s this: “My biopsy showed complete fibrosis reversal.” That’s the hope. That’s the reward for sticking with a tough treatment plan.
And here’s the sobering stat: 65% of patients say steroid side effects are worse than the disease itself. That’s why combination therapy matters. It’s not just about healing the liver - it’s about keeping your quality of life.
What’s Changing in 2026?
The 2025 EASL guidelines are already reshaping practice. No more subclassification. Longer window to assess response (6-12 months, not just 6). Stronger emphasis on biopsy for remission confirmation. And a push for TPMT testing everywhere.
Research is moving fast. Blood tests that predict steroid response within two weeks? MicroRNA panels are showing 85% accuracy. Genetic markers like HLA-DRB1*03:01 are helping identify who’s at highest risk. Personalized treatment isn’t science fiction anymore.
The global AIH market is growing - from $1.2 billion in 2024 to $1.8 billion by 2029. Why? Because more people are being diagnosed. And because treatment is getting smarter.


Kathryn Lenn
February 9, 2026So let me get this straight - we’re giving people powerful immunosuppressants because their body’s being ‘too loyal’ to itself? 🤔 Next they’ll tell us our kidneys are just overachieving. I’ve seen too many people on prednisone turn into inflatable beach toys. This isn’t medicine - it’s a corporate-sponsored hostage situation. And don’t even get me started on that TPMT test. 45% in the US? Yeah, right. They’re probably too busy billing for MRIs to care if you live or die.
Frank Baumann
February 11, 2026I had autoimmune hepatitis for seven years before I got diagnosed - and honestly? I thought I was just ‘tired all the time’ until my ALT hit 1200. I was 32. I had a 2-year-old. My wife cried in the ER. Prednisone made me look like a balloon animal - moon face, acne, insomnia, mood swings that made me yell at my cat for breathing too loud. But then we added azathioprine. Slow. Painful. Blood tests every week. And then - miracle - at 18 months, my biopsy showed F0. No scarring. I’m off steroids now. I lift weights. I sleep through the night. This isn’t just science. It’s a second chance. Don’t give up. Even if your face looks like a Thanksgiving turkey.
Marie Fontaine
February 12, 2026Yessss this is so important!! 🙌 I was diagnosed last year and honestly? I was terrified. But my doc did the TPMT test right away - THANK GOD - and we started low and slow. Now I’m on 5mg prednisone and 75mg azathioprine. My liver enzymes are NORMAL. I even started hiking again!! 💪 If you’re scared? You’re not alone. But it DOES get better. You CAN heal. I’m living proof!! ❤️
Lyle Whyatt
February 12, 2026I’ve been managing AIH for over a decade now - and I’ve watched the guidelines shift like sand. The 2025 EASL move to drop Type 1/Type 2? Brilliant. Who cares if you have ANA or LKM1? You still get crushed by the same immune attack. The real breakthrough? The push for histological remission. Too many docs stop at normal enzymes. But fibrosis doesn’t vanish just because your ALT drops. You need the biopsy. Repeat it. Don’t trust the numbers alone. I had F3 fibrosis. Now? F0. Took three years. But I’m here. And I’m not just surviving - I’m thriving. That’s the goal.
Tasha Lake
February 14, 2026The IgG threshold of ≥1.5x ULN is clinically significant because it reflects polyclonal B-cell activation - a hallmark of T-helper 17-mediated liver inflammation. Coupled with interface hepatitis on biopsy, which indicates lymphocytic infiltration at the portal-parenchymal junction, this creates a diagnostic triad that’s highly specific when viral etiologies are excluded. The revised IAIHG scoring system’s sensitivity and specificity exceed 90% in validated cohorts. TPMT genotyping remains underutilized in community practice, despite its predictive value for myelotoxicity - a class I recommendation per EASL 2025.
Sam Dickison
February 15, 2026Man, I wish I’d known about TPMT before I started azathioprine. I went full panic mode when my WBC dropped to 2.1. Turns out I’m a slow metabolizer. My doc had to switch me to mycophenolate. Took 6 months to stabilize. But hey - no more moon face. No more 3 a.m. panic attacks. Just regular bloodwork and a lot of patience. If you’re on this journey? Don’t rush the taper. And get those hep A/B shots BEFORE you start. Seriously. Don’t be me.
Brett Pouser
February 15, 2026I’m from rural Alabama. No liver specialist within 150 miles. My local doc just said ‘take the pills’ and sent me on my way. I didn’t know about TPMT testing until I found a Reddit thread. I paid out of pocket. $300. Worth every penny. Now I’m on mycophenolate. No pancreatitis. No crashes. Just… life. People in places like mine need access to this info. Not everyone’s got a hospital with a hepatology department. This stuff saves lives - but only if you know it exists.
Simon Critchley
February 16, 2026Let’s be real - prednisone is basically a chemical version of a middle finger from your own immune system. 🤬 And azathioprine? It’s the quiet assassin. Slow, sneaky, but it gets the job done. I’ve seen patients go from ‘I can’t walk up the stairs’ to ‘I ran a 10K last weekend’ on this combo. But here’s the kicker - the FDA’s backing obeticholic acid? That’s the real game-changer. 42% complete response? That’s not a trial. That’s a revolution. Next decade? We’ll be talking about AIH like we talk about diabetes. Manageable. Predictable. Human.
Karianne Jackson
February 17, 2026I gained 40 pounds in 2 months. My face looked like a balloon. I cried every night. I hated my body. I wanted to quit. But I didn’t. And now? I’m off everything. My liver is fine. It’s not magic. It’s medicine. And you can do it too.
Tom Forwood
February 19, 2026yo so i got diagnosed last year and honestly i was scared outta my mind. my doc was like ‘take this pill’ and i was like ‘wait what if i die?’ but then i found this subreddit and learned about tpmt testing. i got it done. turned out i was a slow metabolizer. switched to myco. now i’m on 5mg prednisone and 1g mycophenolate. no pancreatitis. no moon face. just… me. and i’m alive. and i’m happy. and i’m not alone. you’re not alone either. 💙
Chelsea Cook
February 20, 2026Oh, so now we’re supposed to be grateful that steroids make us look like a Michelin Man while we’re trying to hold down our lunch? Classic. And azathioprine? Yeah, because nothing says ‘I love you’ like pancreatitis. But hey - at least we’re not being told to ‘just eat less sugar’ like it’s a lifestyle blog. We’re fighting a war inside our own bodies. And yeah - the science works. But it shouldn’t cost us our dignity.
John Sonnenberg
February 20, 2026I’ve read this article three times. I’ve checked the references. I’ve called three specialists. And I’m still not convinced. Why are we assuming the immune system is ‘wrong’? What if it’s not attacking - what if it’s trying to heal? What if the liver is signaling distress and we’re silencing the messenger? What about gut microbiome dysbiosis? What about environmental toxins? Why is no one talking about epigenetics? Why is the only solution to suppress? We’re treating symptoms - not causes. And that’s not medicine. That’s avoidance.
Jessica Klaar
February 21, 2026I’m so glad someone finally put this out there. I was diagnosed 8 years ago. I was 28. I had two kids. I thought I was dying. I lost my job. I lost friends. But I didn’t lose hope. We tried everything. Steroids made me feel like a ghost. Azathioprine made me nauseous. Mycophenolate? Finally, a lifeline. My biopsy went from F3 to F0. I’m off meds now. I run marathons. I coach my daughter’s soccer team. It’s not a miracle. It’s persistence. And yes - TPMT testing saved my life. Please, if you’re reading this - ask for it. Demand it. Don’t let them skip it.
Patrick Jarillon
February 21, 2026Let me guess - this is all funded by Big Pharma. Prednisone? Azathioprine? Mycophenolate? All patented. All expensive. Meanwhile, the real cause - glyphosate, EMFs, vaccines, water fluoridation - is being buried. You think they want you to heal? No. They want you dependent. They want you on lifelong meds. They want you coming back every month. That biopsy? That’s just a money-maker. The ‘remission’? A placebo effect. Wake up. There’s a reason they banned TPMT testing in 3 countries. This isn’t science. It’s control.